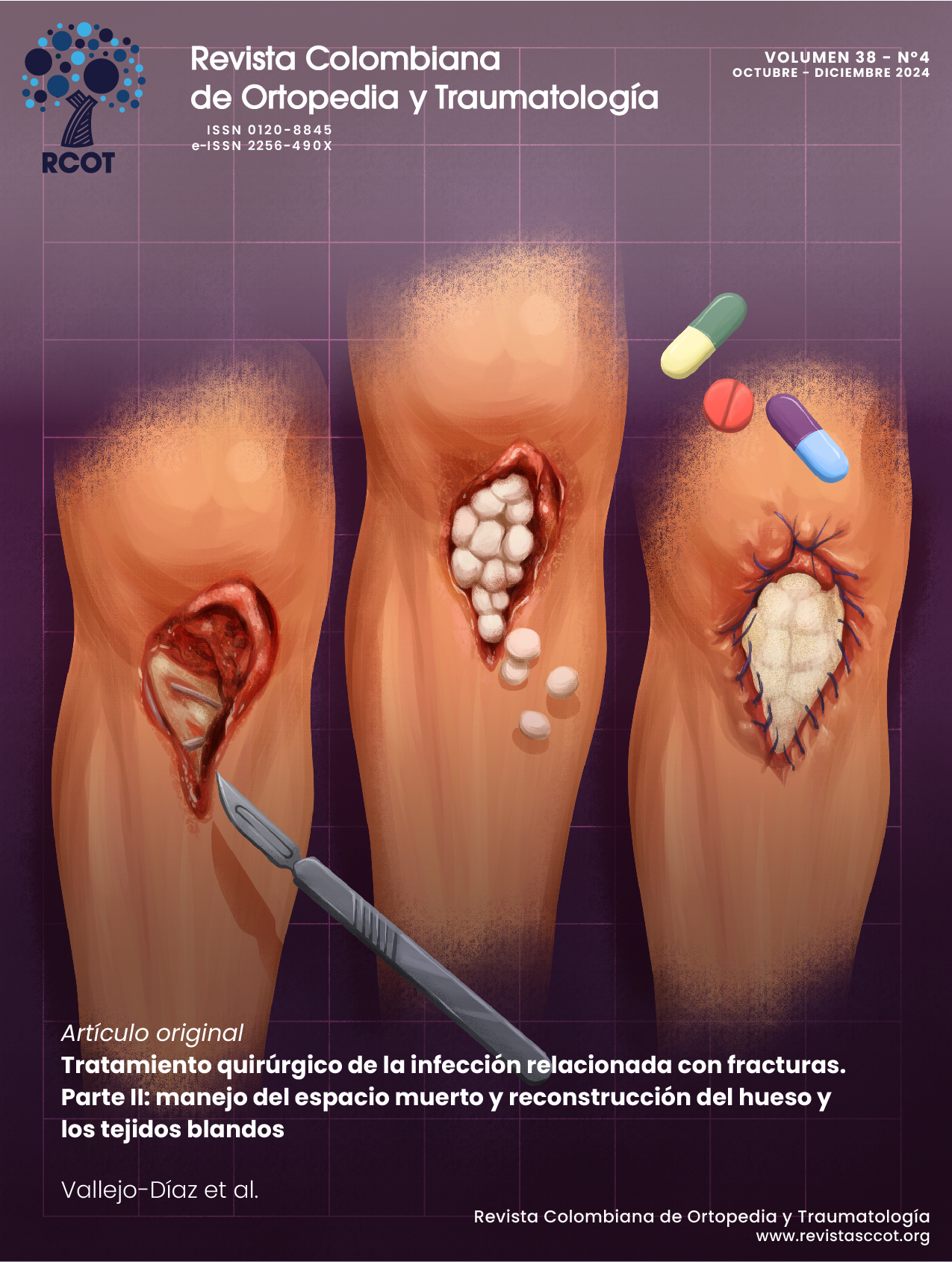
Tratamiento quirúrgico de la infección relacionada con fracturas. Parte II: manejo del espacio muerto y reconstrucción del hueso y los tejidos blandos
DOI:
https://doi.org/10.58814/01208845.87Palabras clave:
Osteomielitis, Fracturas óseas, Fijación interna de fracturas, infección de la herida quirúrgicaResumen
El desbridamiento es la piedra angular del tratamiento de la infección relacionada con fracturas e implica la escisión de todo el tejido necrótico e infectado. Desafortunadamente, el desbridamiento de huesos y tejidos blandos con frecuencia resulta en espacio muerto, defectos óseos y defectos en tejidos blandos. Por lo tanto, inmediatamente después del desbridamiento es necesario planificar las estrategias quirúrgicas reconstructivas. Teniendo en cuenta lo anterior, el objetivo de este artículo es revisar las técnicas quirúrgicas disponibles para el manejo del espacio muerto y la reconstrucción ósea y de tejidos blandos en pacientes con infección relacionada con fracturas.
Descargas
Referencias bibliográficas
Metsemakers WJ, Morgenstern M, McNally MA, Moriarty TF, McFadyen I, Scarborough, et al. Fracture-related infection: A consensus on definition from an international expert group. Injury. 2018;49(3):505-10. https://doi.org/gdcrpb.
Metsemakers WJ, Morgenstern M, Senneville E, Borens O, Govaert GAM, Onsea J, et al. General treatment principles for fracture-related infection: recommendations from an international expert group. Arch Orthop Trauma Surg. 2020;140(8):1013-27. https://doi.org/ghmfvw.
Azi ML, Kojima KE, Pesántez R, Carabelli G, Borens O, McFadyen I, et al. Effectiveness of an Online Course on Fracture-Related Infections. J Eur CME. 2022;11(1): 2024682. https://doi.org/nth8.
Azi ML, Valderrama-Molina CO, Vallejo-Diaz A, et al. Tratamiento quirúrgico de la infección relacionada con fracturas Parte I: desbridamiento óseo y de tejidos blandos. Rev Col Or Tra. 2024;38(1): e57. https://doi.org/nth9.
Gage MJ, Yoon RS, Gaines RJ, Dunbar RP, Egol KA, Liporace FA. Dead Space Management After Orthopaedic Trauma: Tips, Tricks, and Pitfalls. J Orthop Trauma. 2016;30(2):64-70. https://doi.org/f782j7.
Metsemakers WJ, Fragomen AT, Moriarty TF, Morgenstern M, Egol KA, Zalavras C, et al. Evidence-Based Recommendations for Local Antimicrobial Strategies and Dead Space Management in Fracture-Related Infection. J Orthop Trauma. 2020;34(1):18-29. https://doi.org/ghx7c3.
Jaeblon T. Polymethylmethacrylate: properties and contemporary uses in orthopaedics. J Am Acad Orthop Surg. 2010;18(5):297-305. https://doi.org/f3v9xf.
Eikani C, Hoyt A, Cho E, Levack AE. The State of Local Antibiotic Use in Orthopedic Trauma. Orthop Clin North Am. 2024;55(2):207-16. https://doi.org/ntjb.
Schnettler R, Steinau HU, Adams S. Septic bone and joint surgery. Stuttgart: Thieme; 2010.
Hake ME, Young H, Hak DJ, Stahel PF, Hammerberg EM, Mauffrey C. Local antibiotic therapy strategies in orthopaedic trauma: Practical tips and tricks and review of the literature. Injury. 2015;46(8):1447-56. https://doi.org/f7s9cp.
Samuel S, Ismavel R, Boopalan PR, Matthai T. Practical considerations in the making and use of high-dose antibiotic-loaded bone cement. Acta Orthop Belg. 2010;76(4):543-5.
Berberich C, Kuhn KD, Alt V. Knochenzement als lokaler Antibiotikaträger [Bone cement as a local antibiotic carrier]. Orthopadie (Heidelb). 2023;52(12):981-1. https://doi.org/ntjc.
Neut D, van de Belt H, Stokroos I, van Horn JR, van der Mei C, Busscher HJ. Biomaterial-associated infection of gentamicin-loaded PMMA beads in orthopaedic revision surgery. J Antimicrob Chemother. 2001;47(6):885-91. https://doi.org/dtkk5w.
Ganta A, Merrell LA, Adams J, Konda SR, Egol KA. Retention of Antibiotic Cement Delivery Implants in Orthopedic Infection Associated With United Fractures Does Not Increase Recurrence Risk. J Orthop Trauma. 2024;38(4):190-5. https://doi.org/ntjd.
Ge SM, Harvey EJ. Collagen fleece in orthopaedic infections. OTA Int. 2021;4(Suppl 3):e111(1-5). https://doi.org/ntkk.
Malizos K, Blauth M, Danita A, Capuano N, Mezzoprete R, Logoluso N, et al. Fast-resorbable antibiotic-loaded hydrogel coating to reduce post-surgical infection after internal osteosynthesis: a multicenter randomized controlled trial. J Orthop Traumatol. 2017;18(2):159-69. https://doi.org/gn73ch.
Robert N. Negative pressure wound therapy in orthopaedic surgery. Orthop Traumatol Surg Res. 2017;103(1S):S99-S103. https://doi.org/gc5wq5.
Sweere V, Sliepen J, Haidari S, Depypere M, Mertens M, Ijpma F, et al. Use of negative pressure wound therapy in patients with fracture-related infection more than doubles the risk of recurrence. Injury. 2022;53(12):3938-44. https://doi.org/ntkm.
Haidari S, FFA IJ, Metsemakers WJ, Maarse W, Vogely HC, Ramsden AJ, et al. The Role of Negative-Pressure Wound Therapy in Patients with Fracture-Related Infection: A Systematic Review and Critical Appraisal. Biomed Res Int. 2021;2021:7742227. https://doi.org/gsj32r.
Sharr J, Rizos J, Buckley R. Negative pressure wound therapy in orthopedic trauma - is it an efficacious tool or just convenient? Injury. 2023:S0020-1383(23)00354-6. https://doi.org/ntmg.
Rupp M, Walter N, Szymski D, Taeger C, Lager MF, Alt V. The antibiotic bead pouch - a useful technique for temporary soft tissue coverage, infection prevention and therapy in trauma surgery. J Bone Jt Infect. 2023;8(3):165-73. https://doi.org/ntmh.
Henry SL, Ostermann PA, Seligson D. The antibiotic bead pouch technique. The management of severe compound fractures. Clin Orthop Relat Res. 1993;(295):54-62.
Prasarn ML, Zych G, Ostermann PA. Wound management for severe open fractures: use of antibiotic bead pouches and vacuum-assisted closure. Am J Orthop (Belle Mead NJ). 2009;38(1):559-63.
Bidolegui F, Codesido M, Pereira S, Abraham A, Esteves RP, Giordano V. Antibiotic cement-coated plate is a viable and efficient technique for the definitive management of metaphyseal septic nonunions of the femur and tibia. Rev Col Bras Cir. 2023;49:e20223060. https://doi.org/ntmj.
Zalikha AK, Sayeed Z, Stine SA, Bray R, Vaidya R. Antibiotic Cement-Coated Interlocked Intramedullary Nails for the Treatment of Infected Nonunion After Intramedullary Nailing. J Orthop Trauma. 2023;37(1):e1-e6. https://doi.org/ntmk.
Moghaddam A, Weis J, Haubruck P, Raven TF, Addali A, Schmidmaier G. Evaluation of the clinical use of the ETN PROtect(R) in non-union therapy. Injury. 2019;50(Suppl 3):32-9. https://doi.org/ntmm.
Walter N, Popp D, Freigang V, Nerlich M, Alt V, Rupp M. Treatment of severely open tibial fractures, non-unions, and fracture-related infections with a gentamicin-coated tibial nail-clinical outcomes including quality of life analysis and psychological ICD-10-based symptom rating. J Orthop Surg Res. 2021;16:270. https://doi.org/nw7c.
Parsons B, Strauss E. Surgical management of chronic osteomyelitis. Am J Surg. 2004;188(Suppl 1A):57-66. https://doi.org/bmtmdw.
Azoury SC, Kovach SJ, Levin LS. Reconstruction Options for Lower Extremity Traumatic Wounds. J Am Acad Orthop Surg. 2022;30(16):735-46. https://doi.org/nw7d.
d'Avila F, Franco D, d'Avila B, Arnaut MJ. Use of local muscle flaps to cover leg bone exposures. Rev Col Bras Cir. 2014;41(6):434-9. https://doi.org/nw7f.
Hong JPJ, Goh TLH, Choi DH, Kim JJ, Suh HS. The Efficacy of Perforator Flaps in the Treatment of Chronic Osteomyelitis. Plast Reconstr Surg. 2017;140(1):179-88. https://doi.org/gbmttd.
Friedrich JB, Katolik LI, Hanel DP. Reconstruction of soft-tissue injury associated with lower extremity fracture. J Am Acad Orthop Surg. 2011;19(2):81-90. https://doi.org/f3wfbz.
Persaud S, Chesser A, Pereira R, Ross A. Sural Flap Use for the Treatment of Wounds With Underlying Osteomyelitis: Graft Size a Predictor in Outcome, a Systematic Review. Foot Ankle Spec. 2017;10(6):560-66. https://doi.org/nw7g.
Müller SLC, Morgenstern M, Kuehl R, Muri T, Kalbermatten DF, Class M, et al. Soft-tissue reconstruction in lower-leg fracture-related infections: An orthoplastic outcome and risk factor analysis. Injury. 2021;52(11):3489-97. https://doi.org/nw7h.
Nauth A, Schemitsch E, Norris B, Nollin Z, Watson JT. Critical-Size Bone Defects: Is There a Consensus for Diagnosis and Treatment? J Orthop Trauma. 2018;32(Suppl 1):S7-S11. https://doi.org/gqnt3n.
Bezstarosti H, Metsemakers WJ, van Lieshout EMM, Voskamp LW, Kortram K, McNally MA, et al. Management of critical-sized bone defects in the treatment of fracture-related infection: a systematic review and pooled analysis. Arch Orthop Trauma Surg. 2021;141(7):1215-30. https://doi.org/gj8k2b.
Liu K, Jia Q, Wang X, Bahesutihan Y, Ma C, Ren P, et al. Complications associated with single-level bone transport for the treatment of tibial bone defects caused by fracture-related infection. BMC Musculoskelet Disord. 2023;24:514. https://doi.org/nw7j.
Geurts J, Chris Arts JJ, Walenkamp GH. Bone graft substitutes in active or suspected infection. Contra-indicated or not? Injury. 2011;42(Suppl 2):S82-86. https://doi.org/cs6s3p.
Kojima KE, de Andrade ESFB, Leonhardt MC, Cordeiro de Carvalho V, Domingos de Oliverira PR, Munhoz Lima ALL, et al. Bioactive glass S53P4 to fill-up large cavitary bone defect after acute and chronic osteomyelitis treated with antibiotic-loaded cement beads: A prospective case series with a minimum 2-year follow-up. Injury. 2021;52(Suppl 3):S23-S28. https://doi.org/gkbtk4.
Ferrando A, Part J, Baeza J. Treatment of Cavitary Bone Defects in Chronic Osteomyelitis: Biogactive glass S53P4 vs. Calcium Sulphate Antibiotic Beads. J Bone Jt Infect. 2017;2(4):194-201. https://doi.org/nw7m.
Romano CL, Logoluso N, Meani E, Romano D, De Vecchi E, Vassena C, et al. A comparative study of the use of bioactive glass S53P4 and antibiotic-loaded calcium-based bone substitutes in the treatment of chronic osteomyelitis: a retrospective comparative study. Bone Joint J. 2014;96-B(6):845-50. https://doi.org/nw7p.
Migliorini F, La Padula G, Torsiello E, Spieza F, Oliva F, Maffulli N. Strategies for large bone defect reconstruction after trauma, infections or tumour excision: a comprehensive review of the literature. Eur J Med Res. 2021;26(1):118. https://doi.org/gt6tdm.
Ferreira N, Tanwar YS. Systematic Approach to the Management of Post-traumatic Segmental Diaphyseal Long Bone Defects: Treatment Algorithm and Comprehensive Classification System. Strategies Trauma Limb Reconstr. 2020;15(2):106-16. https://doi.org/nw7q.
Dawson J, Kiner D, Gardner 2nd W, Swafford R, Nowotarski PJ. The reamer-irrigator-aspirator as a device for harvesting bone graft compared with iliac crest bone graft: union rates and complications. J Orthop Trauma. 2014;28(10):584-90. https://doi.org/f6jq5h.
Tsang SJ, Ferreira N, Simpson A. The reconstruction of critical bone loss: the holy grail of orthopaedics. Bone Joint Res. 2022;11(6):409-12. https://doi.org/nw7r.
Kadhim M, Holmes L Jr, Gesheff MG, Conway JD. Treatment Options for Nonunion With Segmental Bone Defects: Systematic Review and Quantitative Evidence Synthesis. J Orthop Trauma. 2017;31(2):111-19. https://doi.org/f9s8zq.
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2024 Revista Colombiana de ortopedia y traumatología

Esta obra está bajo una licencia Creative Commons Reconocimiento 3.0 Unported.