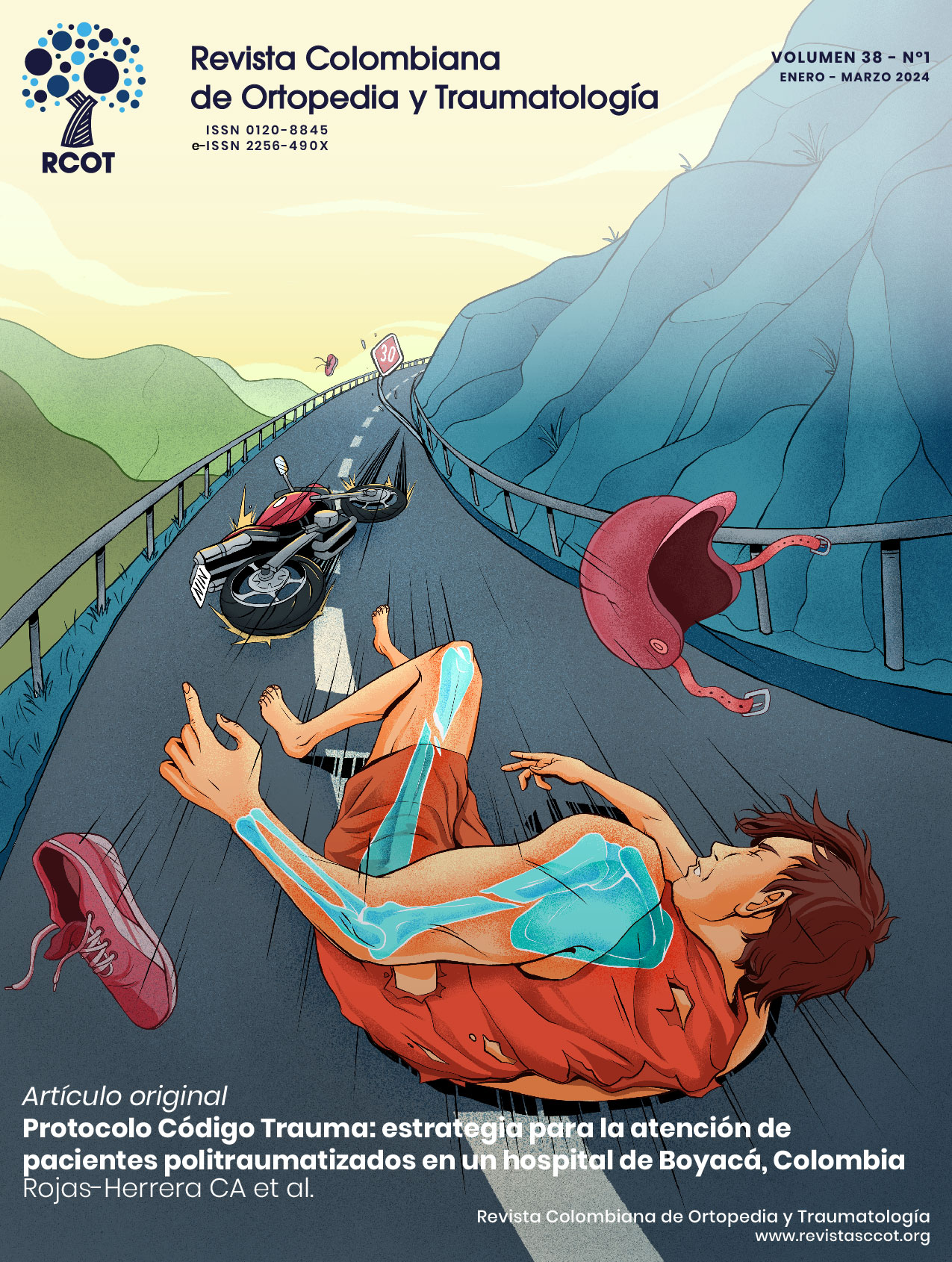
Trauma Code Protocol: a useful tool for the management of polytraumatized patients at a hospital in Boyacá, Colombia
DOI:
https://doi.org/10.58814/01208845.68Keywords:
Multiple Trauma, Cross-Sectional Studies, Clinical protocols, Emergencies, MortalityAbstract
Introduction: Polytrauma is the leading cause of death and disability in people <35 years of age, so it is necessary to develop and implement multidisciplinary protocols for their treatment. The Trauma Code Protocol is an interdisciplinary strategy designed to optimize the management of polytraumatized patients and reduce their mortality.
Objective: To describe the sociodemographic and clinical characteristics of polytraumatized patients treated at a hospital in Boyacá (Colombia) using the Trauma Code Protocol.
Methodology: Cross-sectional descriptive study conducted in 100 patients treated at the emergency room of a university hospital in Tunja (Colombia) between 2020 and 2022 using a specific protocol for the management of polytraumatized patients.
Results: The median age of the participants was 34.5 years, 79% were male (95%CI: 70.0-85.8%), and 44% were treated in 2022. The most frequent treating specialties were orthopedics and trauma (69%), neurosurgery (57%), and general surgery (36%). Moreover, the most common diagnoses were head trauma (46%; 95%CI: 36.5-55.7%) and blunt trauma of the chest (n=28; 95%CI: 20.1-37.4%) or abdomen (n=26; 95%CI: 18.4-35.3%). The median values for hemoglobin, pH, base excess, and lactate levels were 12.3g/dL, 7.34, -7.90mEq/L, and 3.84 mmol/L, respectively. The median time between activation of the Severe Trauma Team Protocol and surgery was 112 minutes. Finally, 71% of patients survived (95%CI: 61.4-78.9%).
Conclusion: The Trauma Code Protocol is a useful strategy for the management of polytraumatized patients, particularly regarding the early identification of the patient's sociodemographic and clinical characteristics and its multidisciplinary approach.
Downloads
References
Trujillo-Trejos I, Gutiérrez-Calderón ES, Giraldo-Castañeda EL, Grisales-Giraldo GA, Agudelo-Suárez AA. Lesiones por accidentes de tránsito en una institución de salud en el municipio de Pereira entre los años 2014-2017. Univ Salud. 2018;21(1):8-18. https://doi.org/mtht.
Alberdi F, García I, Atutxa L, Zabarte M, Trauma and Neurointensive Care Work Group of the SEMICYUC. Epidemiology of severe trauma. Med Intensiva. 2014;38(9):580-8. https://doi.org/f2wghj.
Dijkink S, van der Wilden GM, Krijnen P, Dol L, Rhemrev S, King DR, et al. Polytrauma patients in the Netherlands and the USA: A bi-institutional comparison of processes and outcomes of care. Injury. 2018;49(1):104-9. https://doi.org/gcv3z4.
Wong K, Petchell J. Trauma teams in Australia: a national survey. ANZ J Surg. 2003;73(10):819-25. https://doi.org/bghbzx.
Fischer A, Fitzgerald M, Curtis K, Balogh ZJ. The Australian Trauma Registry (ATR): a leading clinical quality registry. Eur J Trauma Emerg Surg. 2023;49(4):1639-45. https://doi.org/mthv.
Hafez AT, Omar I, Aly M. Challenges to the development of the trauma system in Egypt. J Public Health Afr. 2023;14(5):2214. https://doi.org/mthw.
Candefjord S, Asker L, Caragounis EC. Mortality of trauma patients treated at trauma centers compared to non-trauma centers in Sweden: a retrospective study. Eur J Trauma Emerg Surg. 2022;48(1):525-36. https://doi.org/gh9mgg.
Departamento Administrativo Nacional de Estadística (DANE). Boletín técnico. Estadísticas Vitales (EEVV). Defunciones fetales y no fetales (IV trimestre 2022pr, acumulado 2022pr y año corrido 2023pr). Bogotá D.C: (DANE); marzo 24 2023. Available from: https://bit.ly/3yqQuzX.
Uribe FL, Carvajal SM, Torres NF, Bustamante LA, García AF. Equipos de trauma: realidad mundial e implementación en un país en desarrollo. Descripción narrativa. Rev Colomb Cir. 2021;36(1):42-50. https://doi.org/mth3.
Rossaint R, Afshari A, Bouillon B, Cerny V, Cimpoesu D, Curry N, et al. The European guideline on management of major bleeding and coagulopathy following trauma: sixth edition. Crit Care. 2023;27(1):80. https://doi.org/mth4.
Turculeţ CŞ, Georgescu TF, Iordache F, Ene D, Gaşpar B, Beuran M. Polytrauma: The European Paradigm. Chirurgia (Bucur). 2021;116(6):664-8. https://doi.org/mth5.
American College of Surgeons. Advanced Trauma Life Support (ATLS). Student Course Manual. 10th ed. Chicago: American College of Surgeons; 2018.
Callaway DW, Shapiro NI, Donnino MW, Baker C, Rosen CL. Serum lactate and base deficit as predictors of mortality in normotensive elderly blunt trauma patients. J Trauma. 2009;66(4):1040-44. https://doi.org/dq2qz7.
Régnier MA, Raux M, Le Manach Y, Asencio Y, Gaillard J, Devilliers C, et al. Prognostic significance of blood lactate and lactate clearance in trauma patients. Anesthesiology. 2012;117(6):1276-88. https://doi.org/f4d9v8.
World Medical Association (WMA). WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Fortaleza: 64th WMA General Assembly; 2013.
Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993 [cited 2024 May 07]. Available from: https://bit.ly/31gu7do.
Hofman M, Sellei R, Peralta R, Balogh Z, Wong TH, Evans JA, et al. Trauma systems: models of prehospital and inhospital care. Eur J Trauma Emerg Surg. 2012;38(3):253-60. https://doi.org/mth8.
Montoya L, Kool B, Dicker B, Davie G. Epidemiology of major trauma in New Zealand: a systematic review. N Z Med J. 2022;135(1550):86-110.
Kazemi AR, Nayeem N. The existence and composition of Trauma Teams in the UK. Injury. 1997;28(2):119-21. https://doi.org/bjhf4h.
Kashani P, Saberinia A. Management of multiple traumas in emergency medicine department: A review. J Family Med Prim Care. 2019;8(12):3789-97. https://doi.org/mth9.
Hokema F, Donaubauer B, Busch T, Bouillon B, Kaisers U. Schockraummanagement nach dem ATLS-Algorithmus [Initial management of polytraumatized patients in the emergency department]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2007;42(10):716-23. https://doi.org/d7zdqj.
Shatney CH. Resuscitation and evaluation of victims of blunt multisystem trauma. Acta Anaesthesiol Belg. 1987;38(4):267-74.
Reicks P, Thorson M, Irwin E, Byrnes MC. Reducing complications in trauma patients: use of a standardized quality improvement approach. J Trauma Nurs. 2010;17(4):185-90. https://doi.org/mtjb.
Moratalla CG, Gómez-Pérez R, Hinojosa-Arco LC, Ocaña-Wilhelmi L. Protocolo del Código Trauma en hospital de nivel III. Cir Andal. 2019;30(1):107-12.
Díaz Vega NA, Sosa Bernal OE. Anuario Territorial de Siniestralidad Vial Boyacá 2021. Bogotá D.C.: 2022 [cited 03 May 2024] Available from: https://bit.ly/3WjN8sp.
Solano-Arboleda N, Rojas AB. Uso de los gases arteriales en trauma. Rev Colomb Cir. 2021;36(1):20-4. https://doi.org/mtjc.
Tovmassian D, Hameed AM, Ly J, Pathmanathan N, Devadas M, Gomez D, et al. Process measure aimed at reducing time to haemorrhage control: outcomes associated with Code Crimson activation in exsanguinating truncal trauma. ANZ J Surg. 2020;90(4):481-5. https://doi.org/mtjd.
Pothiawala S, Friedericksen M, Civil I. Activating Code Crimson in the emergency department: Expediting definitive care for trauma patients with severe haemorrhage in Singapore. Ann Acad Med Singap. 2022;51(8):502-6. https://doi.org/mtjf.
Pape HC, Halvachizadeh S, Leenen L, Velmahos GD, Buckley R, Giannoudis PV. Timing of major fracture care in polytrauma patients - An update on principles, parameters and strategies for 2020. Injury. 2019;50(10):1656-70. https://doi.org/gqm3d3.
Richards JE, Mazzeffi MA, Massey MS, Rock P, Galvagno SM, Scalea TM. The Bitter and the Sweet: Relationship of Lactate, Glucose, and Mortality after Severe Blunt Trauma. Anesth Analg. 2021;133(2):455-61. https://doi.org/mtjg.
Ouellet JF, Roberts DJ, Tiruta C, Kirkpatrick AW, Mercado M, Trottier V, et al. Admission base deficit and lactate levels in Canadian patients with blunt trauma: Are they useful markers of mortality? J Trauma Acute Care Surg. 2012;72(6):1532-5. https://doi.org/mtjh.
Hilbert P, Hofmann GO, Lefering R, Struck MF. Schockraumhämoglobin. Prädiktor für eine Gerinnungsstörung beim Traumapatienten [Trauma bay haemoglobin level. Predictor of coagulation disorder in major trauma]. Unfallchirurg. 2015;118(7):601-6. https://doi.org/gn329x.
Tiel Groenestege-Kreb D, Van Maarseveen O, Leenen L. Trauma team. Br J Anaesth. 2014;113(2):258-65. https://doi.org/f6ch9p.
Härgestam M, Lindkvist M, Jacobsson M, Brulin C, Hultin M. Trauma teams and time to early management during in situ trauma team training. BMJ Open. 2016;6(1):9911. https://doi.org/f3pxnw.
Ordoñez CA, Parra MW, Holguín A, García C, Guzmán-Rodríguez M, Padilla N, et al. La Tomografía Computarizada Corporal Total es una herramienta segura, efectiva y eficiente en el paciente politraumatizado con inestabilidad hemodinámica. Colomb Med. 2020;51(4):1-8. https://doi.org/mtjj.
Georgiou A, Lockey DJ. The performance and assessment of hospital trauma teams. Scand J Trauma Resusc Emerg Med. 2010;18(1):66. https://doi.org/cqjwnd.
Kristiansen LH, Freund DS, Rölfing JHD, Thorninger R. Trauma team training at a "high-risk, low-incidence" hospital. Dan Med J. 2020;67(3):A03190189.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista Colombiana de ortopedia y traumatología

This work is licensed under a Creative Commons Attribution 3.0 Unported License.