original article
Frequency of anterior knee pain following anterior cruciate ligament reconstruction with bone-tendon-bone autograft
Frecuencia del dolor anterior de rodilla luego de reconstrucción del ligamento cruzado anterior con autoinjerto hueso-tendón-hueso
Edgar Alberto Muñoz-Vargas1, Gustavo Andrés Rincón-Plata1,2, Carlos Eduardo Pardo-Laverde1, Luis Alfonso Pinzón-Páez1, Carlos Alfonso Rodríguez-Pinedo1, Alejandro Jesús Fernández-Cárdenas3, Nicolás Barreto-Forero1
1 Hospital de San José, Sociedad de Cirugía de Bogotá, Bogotá D.C., Colombia.
2 Hospital de San José, Orthopedics Service, Bogotá D.C., Colombia.
3 Fundación Universitaria de Ciencias de la Salud, Bogotá D.C., Colombia.
Open access
Received: 02/08/2022
Accepted: 22/12/2022
Corresponding author: Nicolás Barreto Forero. Email: nebarreto@fucsalud.edu.co.
How to cite: Muñoz-Vargas EA, Rincón-Plata GA, Pardo-Laverde CE, Pinzón-Páez LA, Rodríguez-Pinedo CA, Fernández-Cárdenas AJ, Barreto-Forero N. Frequency of anterior knee pain following anterior cruciate ligament reconstruction with bone-tendon-bone autograft. Rev Col Or Tra. 2023;37(1):e8. English. doi:
https://doi.org/10.58814/01208845.8
Cómo citar: Muñoz-Vargas EA, Rincón-
Plata GA, Pardo-Laverde CE, Pinzón-Páez LA, Rodríguez-Pinedo CA, Fernández-Cárdenas AJ, Barreto-Forero N. [Frecuencia del dolor anterior de rodilla luego de reconstrucción del ligamento cruzado anterior con autoinjerto hueso-tendón-hueso]. Rev Col Or Tra. 2023;37(1):e8. English. doi:
https://doi.org/10.58814/01208845.8
Copyright: ©2023 Sociedad Colombiana de Cirugía Ortopédica y Traumatología. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction. Anterior cruciate ligament (ACL) injury is a common condition worldwide, and one of the surgical techniques used to treat it is arthroscopic reconstruction with bone-tendon-bone (BTB) autograft. However, this technique can result in complications such as anterior knee pain, but its prevalence in Colombia is currently unknown.
Objective. To establish the frequency of anterior knee pain after ACL reconstruction using BTB autograft in patients operated on over a 4-year period at the Hospital San José in Bogotá, Colombia.
Methodology. Descriptive study performed in patients diagnosed with ACL injury and taken to ACL reconstruction surgery using BTB autograft between January 2014 and December 2017. A telephone survey and a clinical assessment were performed to characterize pain in patients presenting with this symptom. Data are described using absolute and relative frequencies, as well as medians and ranges.
Results. A total of 257 patients were included, most of whom were male (87.5%) and young adults (42.4%). The prevalence of anterior knee pain was 11.6%. Moreover, none of the patients operated on in 2014 had anterior knee pain at the time of assessment (at 4 or more years of follow-up).
Conclusions. ACL reconstruction using BTB autograft is a surgical technique that offers outstanding outcomes in terms of functional scales and knee stability. The frequency of anterior knee pain was lower than reported in other studies and was more frequently located at the donor site (lower pole of the patella and anterior tibial tuberosity).
Keywords: Anterior Cruciate Ligament; Anterior Cruciate Ligament reconstruction; Patellofemoral Pain; Bone-Patellar Tendon-Bone grafts (MeSH).
Resumen
Introducción. La ruptura del ligamento anterior cruzado (LCA) es una condición frecuente a nivel global y la reconstrucción artroscópica con autoinjerto de hueso-tendón-hueso (HTH) constituye una de las técnicas quirúrgicas para su tratamiento. No obstante, esta técnica puede generar complicaciones como dolor anterior de rodilla. Actualmente, se desconoce su prevalencia en Colombia.
Objetivo. Determinar la frecuencia de dolor anterior de rodilla luego de la reconstrucción de LCA con autoinjerto HTH en pacientes operados en un periodo de 4 años en el Hospital San José en Bogotá, Colombia.
Metodología. Estudio descriptivo realizado en pacientes con diagnóstico de ruptura del LCA llevados a cirugía de reconstrucción de este ligamento mediante HTH entre enero de 2014 y diciembre de 2017. Se realizó una encuesta telefónica y, en los pacientes con dolor, una valoración clínica para caracterizar dicho dolor. Los datos se describen usando frecuencias absolutas y relativas, así como medianas y rangos.
Resultados. Se incluyeron 257 pacientes, la mayoría de los cuales eran hombres (87,5%) y adultos jóvenes (42,4%). La prevalencia del dolor anterior de rodilla fue 11,6%. Además, ninguno de los pacientes operados en 2014 presentó dolor anterior de rodilla en el momento de la valoración (a 4 o más años de seguimiento).
Conclusiones. La reconstrucción del LCA mediante HTH es una técnica quirúrgica que ofrece excelentes resultados en términos de escalas funcionales y estabilidad de la rodilla. La prevalencia de dolor anterior de rodilla fue inferior a la reportada en otros estudios y se localizó con mayor frecuencia en el sitio donante (polo inferior de la rótula y tuberosidad tibial anterior).
Palabras clave. Ligamento Cruzado Anterior; Reconstrucción del Ligamento Cruzado Anterior; Dolor Patelofemoral; Injertos Hueso-Tendón Rotuliano-Hueso (DeCS).
Introduction
Rupture of the anterior cruciate ligament (ACL) is an injury commonly reported worldwide that causes anterolateral rotatory knee instability and alters its biomechanics, changing its center of rotation during walking and sports activities.1 Consequently, this injury impacts the sports performance and daily activities of the patients who suffer from it. It has also been described that ACL injury can lead to meniscal and chondral lesions if not treated in a timely manner.2,3
Arthroscopic ACL reconstruction is widely accepted as the treatment of choice for anterolateral rotatory knee instability, with good outcomes in terms of knee stability and return to sporting activities.4 This surgical procedure is one of the most common in the field of orthopedics. According to estimates, 250 000 procedures are performed in the United States every year, making it the sixth most common arthroscopic procedure in that country.5 This might be explained by the patients’ desire to return to their daily activities and obtain sports results as soon as possible.
The type of graft that should be used in ACL reconstruction has been a topic of debate among surgeons over the last few decades, and several studies have been published offering recommendations, although they may be contradictory.6 One option for ACL reconstruction is bone-tendon-bone (BTB) autograft, which offers adequate results in terms of knee function and stability. Due to its strength, consolidation rate, and stable fixation, this type of graft has become the standard method for ACL reconstruction in recent years.4,7
One of the complications of ACL reconstruction using the BTB technique is anterior knee pain, with a frequency ranging from 14% to 25% as reported in the literature.2,8-10 However, according to a randomized controlled trial with a 15-year follow-up conducted by Webster et al.,6 the prevalence of this type of pain may be similar to that associated with other ACL reconstruction techniques.
Although anterior knee pain has not been defined as a criterion for ACL reconstruction failure, this symptom has been described as one of the reasons for not indicating the use of the BTB technique in certain patients.4 In addition, several hypotheses have been proposed to explain the causes of anterior knee pain after ACL reconstruction, such as the shape and size of the graft, paratenon closure, rehabilitation schedule, quadriceps or hamstring condition, and presence of knee extension deficits prior to surgery; however, none of these variables has been identified as the sole cause of pain.4,11
In view of the foregoing, the objective of this study is to establish the frequency of anterior knee pain after ACL reconstruction using BTB autograft in patients operated on over a 4-year period at the Hospital San José in Bogotá, Colombia.
Methodology
Study type and population
Descriptive study performed on patients with a diagnosis of anterolateral rotatory knee instability caused by ACL rupture, who were taken to ACL reconstruction surgery at the Hospital San José between January 2014 and December 2017 using the BTB technique, which is described in the following subsection.
Exclusion criteria considered variables that impact the postoperative outcome of a patient diagnosed with an ACL injury, namely:
- Being <16 years old or >60 years old.
- Having chondral lesions, meniscal lesions, or ligament injuries other than the ACL injury.
- Having patellofemoral or femorotibial joint alignment problems.
- History of anterior knee pain prior to injury.
- Having knee osteoarthritis (patellofemoral, femorotibial, or tricompartmental).
- Refusal to participate in the study.
ACL reconstruction surgery using the BTB technique at Hospital San José
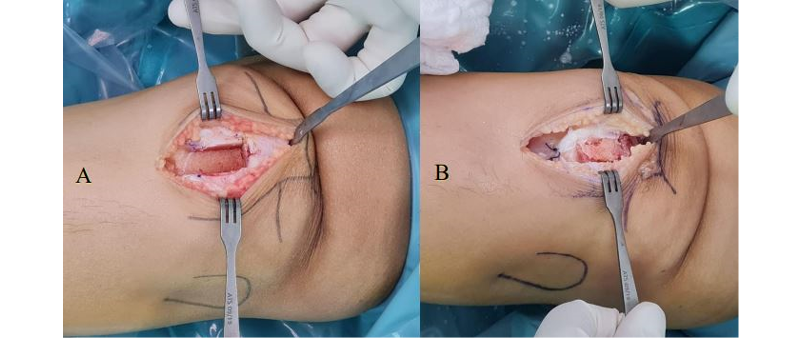
The BTB surgical method developed at our institution has been improved by our surgeons over time. This technique is characterized, firstly, by making only one incision of approximately 4-5cm in length starting 1cm distal to the inferior pole of the patella in a caudal direction (Figure 1), thus avoiding the need to make a double incision and allowing the graft to be taken and mobilized through the tibia by means of the same incision.
Figure 1. Incision of approximately 4-5cm in length in the anterior side of the knee.
Source: Image obtained during the study.
Secondly, harvesting the bone graft from the tibia, which is usually 20mm long, makes it possible to take advantage of the remaining tissue after remodeling the bone plug to place the graft in the defect located in the patella (Figure 2A and 2B).
Figure 2. A) Bone defect in the patella after graft harvesting. B) Bone defect in the patella replaced with autograft obtained in the preparation of bone plugs.
Source: Image obtained during the study.
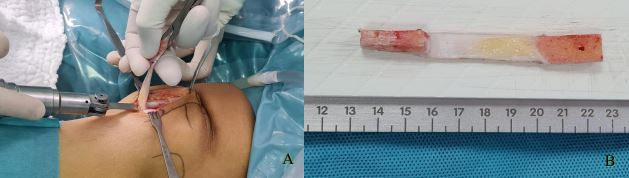
Thirdly, an oscillating saw is used to harvest the graft from the patella (Figure 3A and 3B), trying to avoid the use of chisels or osteotomes, as they may cause bone or cartilage contusions in this bone segment.
Figure 3. A) Graft harvesting with oscillating saw. B) Bone-tendon-bone graft harvested using an oscillating saw.
Source: Image obtained during the study.
Moreover, at the end of the technique, the paratenon is sutured as an independent plane, and the decision whether or not to close the patellar tendon defect is at the surgeon’s discretion (Figure 4).
Figure 4. Independent tendon and paratenon closure.
Source: Image obtained during the study.
In the present study, all patients were discharged on the same day that ACL reconstruction was performed. Finally, after discharge, a generalized rehabilitation plan was implemented, enabling patients to meet certain knee functionality and stability goals within a given time. Adherence to this rehabilitation plan and the achievement of the objectives was verified in postoperative follow-ups.
Procedures and variables
Once the patients were selected based on the inclusion and exclusion criteria, their medical records were reviewed to obtain data regarding their sex and the date the surgery was performed. Furthermore, between September 2018 and September 2019, they were administered a telephone survey in which they were asked about their current age, presence of anterior knee pain (closed question with yes or no answer options), and resumption of their pre-injury work and sports activities. A clinical evaluation was performed on those patients who reported anterior knee pain at the time of telephone contact in order to obtain data on the characteristics of the pain, in particular its location (pain in the patellar or tibial donor site, pain in the patellar tendon region, or functional pain).
It should be noted that pain in the patellar tendon has been associated with the presence of tendinitis after graft harvesting.12,13 Moreover, functional pain was defined as the presence of pain when performing activities that increase pressure in the patellofemoral area, such as standing up from a chair, doing squats, or uphill walking.14
Statistical analysis
Data obtained were tabulated in a Microsoft Excel spreadsheet and described using absolute and relative frequencies for qualitative variables, such as the presence and location of pain, and medians and interquartile ranges for quantitative variables (age) due to the distribution of the data. Statistical analysis was performed in the STATA 13 statistical software.
Ethical considerations
This research followed the ethical principles for conducting biomedical studies involving human subjects established in the Declaration of Helsinki15 and the scientific, technical and administrative standards for health research established in Resolution 8430 of 1993 issued by the Colombian Ministry of Health.17
Results
In total, 520 patients (520 knees) were taken to anterior cruciate ligament reconstruction surgery between January 2014 and December 2017 at Hospital San José. After applying the exclusion criteria, 257 patients (257 knees) were selected to participate in the study.
The majority of participants were male (87.5%), and the median age was 29 years (interquartile range: 23-35 years). Also, most patients were in the 26-35 years age group (42.4%), followed by 16-25 years (33%), 36-45 years (18.7%), and >46 years (5.9%) (Table 1).
Table 1. Demographic characteristics of study participants.
|
Variable
|
Number of patients
(n=257)
|
|
Sex
|
|
Male
Female
|
225 (87.5%)
32 (12.5%)
|
|
Age in years, median (interquartile range)
|
29 (23-35)
|
|
Age group
|
|
16-25 years old
26-35 years old
36-45 years old
>46 years old
|
85 (33%)
109 (42.4%)
48 (18.7%)
15 (5.9%)
|
Source: Own elaboration.
The frequency of anterior knee pain after ACL reconstruction using the BTB technique was 11.67% (Table 2).
Table 2. Frequency of anterior knee pain after ACL reconstruction with BTB autograft by age group.
|
Age group
|
|
Presence of pain
|
16-25 years old
|
26-35 years old
|
36-45 years old
|
>46 years old
|
Total
(n=257)
|
|
No pain
|
78 (91%)
|
94 (86%)
|
41 (86%)
|
14 (93%)
|
227 (88.33%)
|
|
Pain
|
7 (8%)
|
15 (13%)
|
7 (14%)
|
1 (6%)
|
30 (11.67%)
|
Source: Own elaboration.
Pain location was similarly distributed in the donor sites. Specifically, pain in the inferior pole of the patella and in the anterior tibial tuberosity had a frequency of 43.3%. Likewise, pain located in the area of the patellar tendon and functional pain had the same prevalence (6.7%).
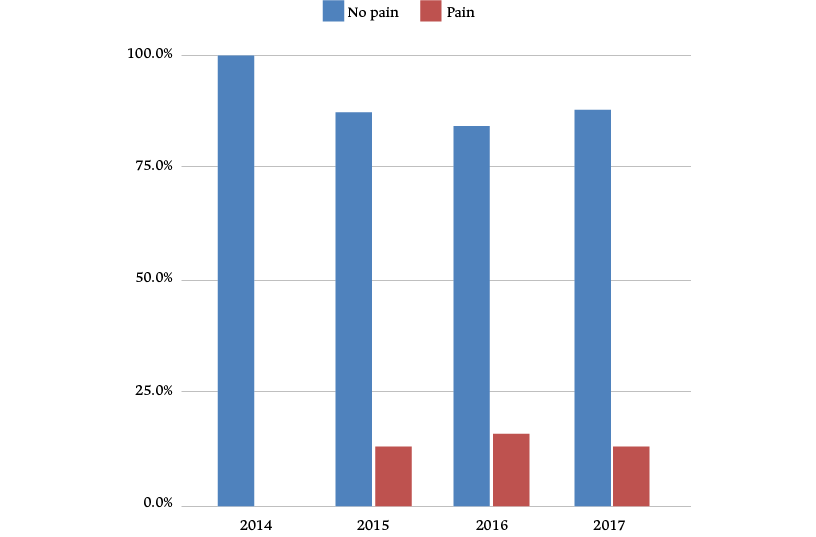
Although the majority of the study participants were men, no differences were observed in the distribution of anterior knee pain between sexes, as the prevalence of pain was 12.5% and 9.3% in men and women, respectively. On the other hand, it was found that patients who underwent surgery in 2014 did not present anterior knee pain at the time of assessment (Figure 5).
Figure 5. Frequency of anterior knee pain after ACL reconstruction with BTB technique by year of surgery.
Source: Own elaboration.
Discussion
Anterior knee pain is one of the complications that should be considered when choosing a surgical technique for ACL reconstruction. Several variables such as location of pain, presence of knee extension deficit, quadriceps function, and time elapsed after surgery should be considered among the causes of its occurrence.9,11,13
In the present study, the prevalence of anterior knee pain was 11.6% in a sample of considerable size (257 patients), a figure relatively lower than that reported in the world literature, in which frequencies between 14% and 25% are described.2,4,8-10 This could be related to the improvement of the surgical technique in our hospital, since the data obtained in the present study do not suggest that the other variables analyzed had an incidence on the occurrence of pain. However, this type of research does not allow us to confirm such a hypothesis.
Other studies have proposed techniques to reduce the incidence of pain after ACL reconstruction by grafting the bone defects.17,18 Despite this, none of those studies have focused on donor site pain and, moreover, no differences have been found in terms of other complications such as re-ruptures or decreased arches of mobility demonstrated on diagnostic imaging or functional scales.10
The surgeons who were involved in this study routinely perform grafting of the patellar defect resulting from graft harvesting. This could be one of the causes of the reduction in the frequency of anterior pain identified in this study, since it has been reported that bone defects resulting from graft harvesting in the patella may be related to the appearance of anterior knee pain.19
The advantage of using the oscillating saw to harvest the graft from the patellar region, both in sagittal and coronal cuts, is avoiding the use of chisels or osteotomes, as well as the impact of the hammer. The surgeons who participated in this study suggest that the use of the oscillating saw reduces the risk of bone contusions at the patella and even patellar fractures.
On the other hand, age was not a variable related to the occurrence of pain; however, the frequency of this symptom in the young adult group (26-35 years: 13%) was higher than in other age groups. This could be related to other variables such as the patient’s activity since, for example, some people with high functional requirements and workloads cannot follow a complete rehabilitation program; these cases should be investigated in further studies.
Pain location is a determining variable in graft selection, as it has been reported that the donor site may present pain on palpation.4,11,20 The results of this study showed that, indeed, pain on palpation of the donor site is more frequent than functional pain and pain in the area of the patellar tendon (caused by tendinitis). This may be related to the time of bone healing at the graft harvest site, which may explain the reason why anterior knee pain was self-limiting and absent 4 years after surgery.
Establishing the characteristics of anterior knee pain is important when evaluating this condition, given that it is not easy to differentiate among studies that distinguish anterior knee pain from pain occurring at the donor site on palpation or from dysesthesia of the infrapatellar branch of the saphenous nerve.21,22 During the course of this study, it was found that some of the patients mistook dysesthesia for anterior knee pain. In this regard, it should be noted that neuritis behaves differently from anterior knee pain in terms of duration.
Although anterior knee pain on palpation at the donor site in cases that have undergone BTB graft has been described as one of the weaknesses of this type of grafting, little research has focused on the long-term follow-up of the results of this technique.6 In the present study, it was observed that anterior knee pain is self-limiting, that is, it disappears some time after the procedure, so there would be no difference with respect to the characteristics of pain reported in patients who have undergone operations involving the use of other types of grafts.6
One of this study’s strengths is that it provides the literature with data on the frequency of anterior knee pain after ACL reconstruction in the Colombian population, since there are few reports on the subject. Moreover, differentiating anterior knee pain from donor site pain is highly relevant, as this aspect has been described as a confounder.20
Limitations of the study include not evaluating patient arches of mobility or intraoperative variables, such as tourniquet use, graft shape, and patellar tendon closure, aspects that could impact the frequency of pain.4,11 However, the results suggest that pain is self-limiting and has no relationship with these variables.
Furthermore, the assessment of the impact of anterior knee pain on activities of daily living is limited, as there is no objective method to quantify this aspect.14 Nevertheless, in the present study, the intensity of anterior knee pain was evaluated by means of visual analog scales, and the results indicate that this symptom did not hinder the performance of everyday or professional activities.6
Finally, it is important to carry out analytical studies at a national level to relate intrinsic variables of the local population to postoperative results, not only concerning the presence and characterization of anterior knee pain, but also the functionality of the knee. Also, these studies could establish the number of procedures performed in Colombia.
Conclusions
ACL reconstruction using BTB autograft is a surgical technique that offers excellent results in terms of functional scales and stability. The prevalence of anterior knee pain was 11.6%, which is relatively lower than other studies, and this pain was most frequently located at the donor site, that is, the inferior pole of the patella and anterior tibial tuberosity.
Despite not having evaluated variables that may impact the presentation of pain, it can be inferred that pain is self-limiting and is not present 4 years after the surgical procedure.
National studies and registries on this subject should be encouraged in order to know the variables of the local population and of this technique that have an impact on the postoperative outcome in the Colombian population.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Zantop T, Petersen W, Sekiya JK, Musahl V, Fu FH. Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):982-92. https://doi.org/b248d5.
2.Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. Clin Orthop Relat Res. 2017;475(10):2459-68. https://doi.org/gbx4bg.
3.Friel NA, Chu CR. The role of ACL injury in the development of posttraumatic knee osteoarthritis. Clin Sports Med. 2013;32(1):1-12. https://doi.org/f4jcj7.
4.Grassi A, Kim C, Marcheggiani-Muccioli GM, Zaffagnini S, Amendola A. What Is the Mid-term Failure Rate of Revision ACL Reconstruction? A Systematic Review. Clin Orthop Relat Res. 2017;475(10):2484-99. https://doi.org/jz29.
5.Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41(10):2439-48. https://doi.org/f5b5xb.
6.Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of Patellar Tendon and Hamstring Tendon Anterior Cruciate Ligament Reconstruction: A 15-Year Follow-up of a Randomized Controlled Trial. Am J Sports Med. 2016;44(1):83-90. https://doi.org/f752kz.
7.Reinhardt KR, Hetsroni I, Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010;41(2):249-62. https://doi.org/cm5zn2.
8.Hirschmann MT, Adler T, Rasch H, Hügli RW, Friederich NF, Arnold MP. Painful knee joint after ACL reconstruction using biodegradable interference screws- SPECT/CT a valuable diagnostic tool? A case report. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:24. https://doi.org/c94rwp.
9.Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22(2):100-10. https://doi.org/f7b56q.
10.Mouarbes D, Menetrey J, Marot V, Courtot L, Berard E, Cavaignac E. Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Outcomes for Quadriceps Tendon Autograft Versus Bone-Patellar Tendon-Bone and Hamstring-Tendon Autografts. Am J Sports Med. 2019;47(14):3531-40. https://doi.org/gqdd58.
11.Niki Y, Hakozaki A, Iwamoto W, Kanagawa H, Matsumoto H, Toyama Y, et al. Factors affecting anterior knee pain following anatomic double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1543-9. https://doi.org/ftkqf9.
12.Shelbourne KD, Trumper RV. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(1):41-7. https://doi.org/b3frn4.
13.Anders JO, Venbrocks RA, Weinberg M. Proprioceptive skills and functional outcome after anterior cruciate ligament reconstruction with a bone-tendon-bone graft. Int Orthop. 2008;32(5):627-33. https://doi.org/brfjjm.
14.Kovindha K, Ganokroj P, Lertwanich P, Vanadurongwan B. Quantifying anterior knee pain during specific activities after using the bone-patellar tendon-bone graft for arthroscopic anterior cruciate ligament reconstruction. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2018;15:6-12. https://doi.org/jz3b.
15.World Medical Association (WMA). WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Fortaleza: 64th WMA General Assembly; 2013.
16.Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993 [cited 2023 Mar 6]. Available from: https://bit.ly/31gu7do.
17.Walters BL, Porter DA, Hobart SJ, Bedford BB, Hogan DE, McHugh MM, et al. Effect of Intraoperative Platelet-Rich Plasma Treatment on Postoperative Donor Site Knee Pain in Patellar Tendon Autograft Anterior Cruciate Ligament Reconstruction: A Double-Blind Randomized Controlled Trial. Am J Sports Med. 2018;46(8):1827-35. https://doi.org/gjgfjb.
18.Boszotta H, Prünner K. Refilling of removal defects: impact on extensor mechanism complaints after use of a bone-tendon-bone graft for anterior cruciate ligament reconstruction. Arthroscopy. 2000;16(2):160-4. https://doi.org/d74dmd.
19.Kartus J, Ejerhed L, Sernert N, Brandsson S, Karlsson J. Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med. 2000;28(3):328-35. https://doi.org/jz3c.
20.Järvelä T, Kannus P, Järvinen M. Anterior knee pain 7 years after an anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Scand J Med Sci Sports. 2000;10(4):221-7. https://doi.org/cwxxhj.
21.Kartus J, Magnusson L, Stener S, Brandsson S, Eriksson BI, Karlsson J. Complications following arthroscopic anterior cruciate ligament reconstruction. A 2-5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):2-8. https://doi.org/frqtxm.
22.Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971-80. https://doi.org/dn6rqk.