Original research
Anatomical reduction and stabilization of acute acromioclavicular dislocation through double-button fixation: clinical and radiological follow-up
Reducción anatómica y estabilización de la luxación acromioclavicular aguda con técnica quirúrgica de doble fijación modificada: seguimiento clínico y radiológico
Andrés Arismendi1 Daniela Galeano2
Daniela Galeano2 Catalina Hurtado2
Catalina Hurtado2 Ana Milena Herrera3
Ana Milena Herrera3
1 Clínica del Campestre, Arm and Shoulder Orthopedic Surgery Service, Medellín, Colombia.
2 Clínica del Campestre, Orthopedics and Priority Consultation Service, Medellín, Colombia.
3 Clínica del Campestre, Epidemiology and Clinical Research Service, Medellín, Colombia.
Open access
Received: 09/05/2022
Accepted: 31/07/2023
Corresponding author: Ana Milena Herrera. Departamento de Epidemiología e Investigación Clínica, Clínica del Campestre, Medellín, Colombia. Email: amht73@gmail.com.
How to cite: Arismendi A, Galeano D, Hurtado C, Herrera AM. Anatomical reduction and stabilization of acute acromioclavicular dislocation through double fixation: clinical and radiological follow-up. Rev Col Or Tra. 2023;37(3):e71. English. doi:
https://doi.org/10.58814/01208845.71
Cómo citar: Arismendi A, Galeano D, Hurtado C, Herrera AM. [Reducción anatómica
y estabilización de la luxación acromioclavicular aguda con técnica quirúrgica de doble fijación modificada: seguimiento clínico y radiológico]. Rev Col Or Tra. 2023;37(3):e71. English. doi:
https://doi.org/10.58814/01208845.71
Copyright: ©2023 Sociedad Colombiana de Cirugía Ortopédica y Traumatología. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction: The treatment of acute acromioclavicular (AC) dislocation using double-button fixation with FiberTape™ and Dog Bone™ neutralized with an AC hook plate (HP) could provide a stable anatomical reduction, resulting in faster rehabilitation and functional recovery.
Objective: To describe short-term radiological and clinical outcomes (minimum one-year of follow-up) achieved with the use of double-button fixation with FiberTape™ and Dog Bone™ neutralized with an AC HP for the surgical treatment of acute AC dislocation.
Methodology: Retrospective study in which the medical records of patients with acute AC dislocation undergoing open anatomic reduction surgery using the modified double- button fixation technique with FiberTape™ and Dog Bone™ between 2017 and 2019 were reviewed. Radiological stability was assessed through the coracoclavicular (CCD) and AC (ACD) distances in the affected and contralateral shoulder. Pain and function were assessed using the visual analogue scale (VAS) and the QuickDASH score, respectively.
Results: Eleven patients were included. The median follow-up was 20 months. AC dislocations were classified as type IV (n=9) and V (n=2) according to the Rockwood classification. An improvement in the median postoperative CDD of the affected shoulder (20.5mm vs. 7.1mm; p=0.000) and ACD (15.2mm vs. 5.1mm; p=0.001) was observed. Moreover, the median CDD of the operated shoulder was 101.9% of the contralateral shoulder. No patient presented with scapular re-luxation or dyskinesia. The median improvement in shoulder function on the QuickDASH score was 19 (p=0.003). Finally, the median VAS score at the last assessment was 1.
Conclusion: The double-button fixation technique provided reliable and stable healing, resulting in early functional recovery with no short-term re-luxation.
Keywords: Acromioclavicular Joint; Joint Dislocations; Joint Instability; Surgical Fixation Devices (MeSH).
Resumen
Introducción. El tratamiento de la luxación acromioclavicular (AC) aguda mediante la técnica quirúrgica de doble fijación con FiberTape™ y botones Dog Bone™ neutralizada con una placa gancho (PG) AC podría permitir una reducción anatómica estable y, por tanto, favorecer una rehabilitación rápida y la recuperación funcional.
Objetivo. Describir los resultados radiológicos y clínicos a corto plazo (mínimo un año de seguimiento) del uso de doble fijación con FiberTape™ y botones Dog Bone™ neutralizada con una PG AC para el tratamiento quirúrgico de la luxación AC aguda.
Metodología. Estudio retrospectivo en el que se revisaron las historias clínicas de pacientes con luxación AC aguda sometidos a cirugía de reducción anatómica abierta utilizando la técnica de doble fijación modificada con FiberTape™ y botones Dog Bone™ entre 2017 y 2019. Se evaluó la estabilidad radiológica a través de las distancias coracoclavicular (DCC) y AC (DAC) en el hombro afectado y el contralateral. El dolor y la funcionalidad se evaluaron mediante la escala visual analóga (EVA) y el cuestionario QuickDASH, respectivamente.
Resultados. Se incluyeron 11 pacientes. La mediana de seguimiento fue 20 meses y las luxaciones AC eran de tipo IV (n=9) y V (n=2) según la clasificación Rockwood. Se evidenció una mejora en las medianas posquirúrgicas de DCC del hombro afectado (20,5mm versus 7,1mm; p=0,000) y DAC (15,2mm versus 5,1mm; p=0,001) Además, la mediana de la DCC del hombro operado fue del 101,9% del hombro contralateral. Ningún paciente presentó reluxaciones o discinesia escapular. La mediana de mejora de la funcionalidad del hombro en la escala QuickDASH fue de 19 (p=0,003). Finalmentela mediana del puntaje EVA en la última evaluación fue 1.
Conclusiones. La técnica con doble fijación proporcionó una cicatrización confiable y estable, así como una pronta recuperación funcional sin reluxaciones a corto plazo.
Palabras clave: Articulación acromioclavicular; Luxaciones articulares; Inestabilidad de la articulación; Dispositivos de fijación quirúrgicos (DeCS).
Introduction
The acromioclavicular (AC) joint is the link between the axial and appendicular skeleton, anchoring the distal clavicle to the acromion of the scapula and also acting as a pivot point between these two bones to stabilize shoulder girdle, facilitating rotation and gliding of the shoulder.1-3 Dynamic and static anatomic structures enable AC joint stability; in particular, static stabilization is maintained by the joint capsule and ligament complex formed by the coracoclavicular (CC), coracoacromial, and AC ligaments, while dynamic stabilization is provided by the trapezius, deltoid, and serratus anterior muscles.2-5
The AC joint has been identified in up to 9% of all shoulder girdle injuries, with a rate of involvement of 1.8 cases per 1 000 injuries per year.1,2 Direct high-energy impact to the lateral aspect of the shoulder or indirect trauma with the arm in adduction that disrupts the ligamentous support of the joint have been reported as the most common mechanisms of injury causing acute high-grade AC joint dislocation.2-4,6 In this regard, early surgical treatment is recommended in patients with type IV, V and VI AC dislocations in the Rockwood classification7 in which there is complete rupture of the CC and AC ligaments.2-4,6
Different open and arthroscopic surgical procedures of anatomic reduction and fixation, as well as ligament reconstruction, have been proposed to achieve AC joint stabilization and realignment.3,4,8,9 However, no consensus has been reached on the best surgical treatment because all reported techniques have advantages and disadvantages. Therefore, obtaining satisfactory results depends mainly on proper patient selection and the surgeon’s experience.2-5,8,9
In 2013, Arismendi et al.10 described a surgical technique combining the use of anchors for CC ligament reconstruction and a hook plate (HP) for AC fixation in 14 patients with type III, IV, and V AC dislocations. In that study, the HP was removed after 12 weeks when the average Constant score was 97. Furthermore, there were no complications during or after surgery, and none of the patients had recurrent dislocation after removing the osteosynthesis material.10 However, it should be noted that although these patients had a satisfactory short-term evolution, the radiological stability of the anatomical reduction was not evaluated.
Since its publication, the technique described by Arismendi et al.10 has evolved, incorporating the reconstruction of the CC ligament with FiberTape™ and Dog Bone™ buttons, and neutralizing this construct with an AC HP. Considering the above, the objective of the present study is to describe the short-term radiological and clinical outcomes (minimum one-year of follow-up) achieved with the use of double-button fixation with FiberTape™ and Dog Bone™ buttons neutralized with an AC HP for the surgical treatment of acute AC dislocation.
Materials and methods
Study design and population
A retrospective study was performed using the clinical data and X-rays of consecutive patients who underwent outpatient surgery for open anatomic reduction of acute AC dislocation with the double-fixation technique at a specialized orthopedic surgery clinic in Medellín, Colombia, between January 2017 and December 2019.
The procedures were performed by the orthopedic surgeon specializing in arm and shoulder care who first described this technique.10 This technique was modified by using a “V-shaped” FiberTape™ construct, as it resembles the anatomy of the conoid and trapezoid ligament, and by fixing this construct with two Dog Bone™ buttons (one used on the clavicle and the other on the coracoid process).
The modified double-fixation technique with the use of FiberTape™ and Dog Bone™ buttons neutralized with an AC HP was used in patients who met the following selection criteria: being between 18 and 60 years old, having type IV or V AC dislocation according to the Rockwood classification,7 and not having vascular or neurological injuries, bilateral dislocations or associated fractures in the affected arm.
The diagnosis of AC dislocation and the Rockwood classification (type IV and V) were achieved based on X-rays (anteroposterior [AP] and Zanca view). All patients underwent surgery within 3 weeks of the trauma. In addition, the QuickDASH score was used to measure the patient’s perception of the functionality of the affected shoulder before surgery.
Surgical technique
The procedure was performed in all patients included in the study as follows: antibiotic prophylaxis with cefazolin (2 grams intravenously) is administered thirty minutes before skin incision. Then, under general anesthesia and using interscalene nerve block, the patient is placed in a beach chair position, and a 5cm longitudinal incision is made on the lateral axis of the clavicle, starting from the dislocated AC joint. Deep dissection follows the deltotrapezial fascia tear at the most lateral aspect of the clavicle and is performed medially through the platysma muscle. The entire clavicle is then dissected, and the dislocated AC joint is completely identified.
Once the traumatic hematoma has been drained, the base of the coracoid process is dissected, its lateral border is released, and a guide wire is placed in the anterior cruciate ligament (ACL) to proceed with drilling below the base of the coracoid process. Next, a small Hohmann retractor is placed on the medial border of the coracoid process. Once the base of the process is visualized without problem, the drill is precisely placed with the ACL guide wire in the middle of the base and the coracoid process is drilled through its superior and inferior cortices. Next, an inferior Dog Bone™ button (Arthrex, Inc., FL, USA), loaded with two FiberTape™ sutures (Arthrex, Inc., FL, USA), is passed retrograde through the perforation. Subsequently, an 18-millimeter-deep LCP® clavicle HP (©DePuy Synthes; Indiana, USA) is temporarily placed, and two holes are drilled in the clavicle, exactly at holes 3 and 4 of the HP shaft. The HP is temporarily removed and FiberTape™ sutures are again passed retrograde through the clavicle through the newly drilled holes, seeking to mimic the anatomy of the trapezoid and conoid ligament. After this, an AC joint reducer is placed and the FiberTape™ is tied over two independent Dog Bone™ buttons over the superior surface of the clavicle. Finally, the 18mm clavicular LCP® HP is definitively placed and fixed with a 3.5mm cortical screw in hole 5 and two locked screws in holes 1 and 2. Then, the incision is closed using absorbable sutures and taking into account the anatomical planes, leaving no vacuum drainage system.
Postoperative care
Ten days after surgery, all patients were assessed, the skin suture and sling were removed, and targeted rehabilitation was indicated. Physical therapy rehabilitation focused on active and passive mobility recovery, involving posterior shoulder capsule elongation for three weeks, as well as, for nine more weeks, general isometric strengthening of the shoulder with TheraBand™ and physical load restriction for the first three weeks. Finally, functional recovery was clinically assessed every three to six months.
Clinical and radiological findings
In the radiological follow-up, X-rays (Zanca view) were used to estimate CCD and ACD in the affected shoulder at three evaluation moments: the immediate postoperative period, three months after the surgical procedure and the last follow-up control, which had to be performed at least 12 months postoperatively. On the other hand, CCD and ACD in the contralateral shoulder were only estimated in the X-ray of the last follow-up.
The CCD was measured from the superior border of the coracoid process to the inferior cortex of the clavicle. The ratio between the CCD of the operated side and the contralateral side was expressed as a percentage, and this allowed classifying the outcome of the anatomic reduction into the following categories: subluxation (>150%), adequate reduction (100-150%), and excessive reduction (<100%). The ACD was measured from the center of the medial aspect of the acromion to the center of the lateral aspect of the clavicle. The presence of heterotopic ossification in the AC and subacromial osteolysis (OS) was also assessed. Measurements were taken by a trained orthopedic resident who had no prior knowledge of the case or previous measurements.
During the last follow-up, OS was estimated and classified according to the criteria of Chang et al.11 into type I (minimal osteolysis), type II (osteolysis: <2 mm), type III (osteolysis: >2 mm), and type IV (osteolysis: cut-through the acromion). Likewise, during the same follow-up, scapular dyskinesia was evaluated, as well as pain using the visual analog scale (VAS) and a subjective assessment of shoulder functionality and satisfaction with the procedure using the QuickDASH questionnaire.
Statistical analysis
Data are described using absolute frequencies and percentages for qualitative variables, and medians and ranges (minimum and maximum values) for quantitative variables, taking into account the non-normal distribution of the data (Shapiro-Wilk test). Statistical analysis was performed in the SPSS software (version 25.0).
The difference between CCD and ACD values in the affected shoulder at the four measurement times (before the procedure and three follow-ups) was evaluated using the Kruskal-Wallis H-test. To compare radiographic measurements between the affected and contralateral shoulder at the last follow-up, the Mann-Whitney U test was used. Finally, to establish the difference in QuickDASH score before and after surgery, the Wilcoxon signed-rank test was used. A statistical significance level of p<0.05 was considered in all statistical tests.
Ethical considerations
The study followed the ethical principles for the conduct of biomedical studies involving human subjects established in the Declaration of Helsinki,12 as well as the scientific, technical and administrative standards for health research contained in Resolution 8430 of 1993 issued by the Colombian Ministry of Health.13 In addition, the study was approved by the Ethics Committee of the institution where the study was conducted as recorded in the minutes of January 15, 2021. It is worth noting that the patients’ identities were kept confidential throughout the study.
Results
Eleven patients were included in the study. The median follow-up time was 20 months (range: 12-39 months), all patients were male, and the median age was 43 years (range: 26-62 years). AC dislocations were classified into types IV and V according to the Rockwood classification in 9 and 2 cases, respectively. Moreover, the median time of HP removal from the clavicle was 17 weeks after surgery (range: 14-26 weeks).
The median preoperative and postoperative QuickDASH scores were 35 (range: 30-44) and 13 (range 11-33), respectively. In addition, the median improvement in the QuickDASH questionnaire score was 19 (range: 8-33; p=0.003). At the last evaluation, the median VAS score was 1 (range: 0-4). There were no cases of re-luxation, scapular dyskinesia, or heterotopic ossification. Finally, the OS was classified as type I in 8 cases and as type II in 3. The characteristics of the patients are described in Table 1.
Table 1. Characteristics of the patients included in the study and postsurgical clinical outcomes.
|
Patient
|
Age
|
Rockwood classification
|
Time to HP removal (in weeks)
|
Time to last follow-up (in months)
|
Pre-surgical QuickDASH score
|
Post-surgical QuickDASH score
|
Post-surgical VAS
|
|
1
|
62
|
V
|
22
|
31
|
32
|
13
|
1
|
|
2
|
33
|
IV
|
26
|
30
|
31
|
11
|
2
|
|
3
|
53
|
IV
|
20
|
12
|
44
|
33
|
0
|
|
4
|
50
|
IV
|
17
|
12
|
41
|
25
|
4
|
|
5
|
36
|
IV
|
15
|
12
|
40
|
23
|
2
|
|
6
|
61
|
IV
|
18
|
39
|
35
|
25
|
2
|
|
7
|
33
|
IV
|
20.5
|
12
|
32
|
11
|
0
|
|
8
|
37
|
IV
|
15
|
36
|
44
|
11
|
3
|
|
9
|
26
|
V
|
15
|
27
|
31
|
11
|
0
|
|
10
|
43
|
IV
|
15
|
20
|
30
|
22
|
0
|
|
11
|
46
|
IV
|
14
|
19
|
44
|
11
|
0
|
VAS: visual analog scale; HP: hook plate.
Source: Own elaboration.
Regarding radiological findings, the median CCD of the affected shoulder was 20.5mm (range: 10-28.7mm) preoperatively, and it improved significantly at each evaluation, with a median of 7.1mm at the last follow-up (range: 4.2-10.2mm; p=0.000). At the last follow-up, the median CCD of the contralateral shoulder was 6.9mm (range: 4.5-12mm), and there was no significant difference between the median CCD of the operated shoulder and the median of the contralateral shoulder (p=0.395). The median postoperative CCD of the operated shoulder was 101.9% of the contralateral shoulder (range: 41.2-177.8%) and 5 cases were classified as over-reductions, 5 as adequate reductions, and 1 as subluxation.
The median ACD of the affected shoulder was 15.2mm (4.9-26.5 mm) before the surgical procedure, 4.45mm (1-7.6 mm) in the immediate postoperative period, 5.2mm (1.2-8.7 mm) at three months, and 5.1 mm (2.9-8.9 mm) at the last follow-up. Importantly, there were statistically significant differences at all evaluation time points (p=0.001). On the other hand, the median ACD of the contralateral shoulder at the last follow-up was 3.4mm (1.8-5.2mm), and there was a statistically significant difference between the median ACD of the operated shoulder and the median ACD of the contralateral shoulder at the last follow-up (p=0.030).
Data on the CCD and ACD are presented in Table 2. Radiological images of one patient were included for illustrative purposes (Figures 1-3).
Table 2. Postsurgical radiological evaluation of the coracoclavicular and acromioclavicular distances.
|
Patient
|
Pre-surgical CCD in AS
|
Postoperative CCD in AS
(in mm)
|
CCD in NAS
|
CCD in AS/ CCD in NAS ratio
|
Anatomical reduction category
|
Pre-surgical ACD in AS
|
Postoperative ACD in AS
(in mm)
|
ACD in NAS
|
|
Immediate
|
3 months
|
Last follow-up
|
Immediate
|
3 months
|
Last follow-up
|
|
1
|
24.8
|
.00
|
.00
|
8.40
|
6.00
|
140.0%
|
Adequate reduction
|
16.6
|
6.00
|
6.00
|
7.60
|
4.20
|
|
2
|
22.3
|
1.90
|
2.60
|
7.13
|
9.80
|
72.8%
|
Over-reduction
|
14.5
|
4.45
|
5.20
|
5.51
|
2.80
|
|
3
|
14.5
|
6.00
|
6.20
|
8.00
|
10.00
|
80.0%
|
Over-reduction
|
11.2
|
2.70
|
2.70
|
4.90
|
2.40
|
|
4
|
12.8
|
.00
|
.00
|
8.00
|
4.50
|
177.8%
|
Subluxation
|
4.9
|
4.00
|
4.00
|
7.00
|
3.60
|
|
5
|
20.5
|
1.20
|
1.90
|
5.40
|
5.30
|
101.9%
|
Adequate reduction
|
16.7
|
4.80
|
4.80
|
2.90
|
1.80
|
|
6
|
16.8
|
3.20
|
7.00
|
7.00
|
5.10
|
137.25%
|
Adequate reduction
|
15.7
|
1.70
|
8.70
|
8.90
|
5.20
|
|
7
|
18.0
|
3.00
|
3.00
|
8.10
|
6.20
|
130.65%
|
Adequate reduction
|
14.5
|
6.00
|
6.20
|
7.50
|
3.70
|
|
8
|
10.0
|
1.20
|
2.00
|
6.40
|
12
|
53.3%
|
Over-reduction
|
7.8
|
1.00
|
1.20
|
4.50
|
3.40
|
|
9
|
28.7
|
2.00
|
3.00
|
5.60
|
6.90
|
81.2%
|
Over-reduction
|
26.5
|
3.20
|
3.20
|
3.20
|
3.70
|
|
10
|
20.5
|
1.80
|
1.80
|
4.20
|
10.20
|
41.2%
|
Over-reduction
|
16.0
|
7.50
|
7.50
|
3.50
|
2.50
|
|
11
|
28.4
|
1.20
|
1.40
|
10.20
|
8.00
|
127.5%
|
Adequate reduction
|
15.2
|
7.60
|
7.60
|
5.10
|
2.30
|
CCD: coracoclavicular distance; ACD: acromioclavicular distance; AS: affected shoulder; NAS: not affected shoulder.
Source: Own elaboration.
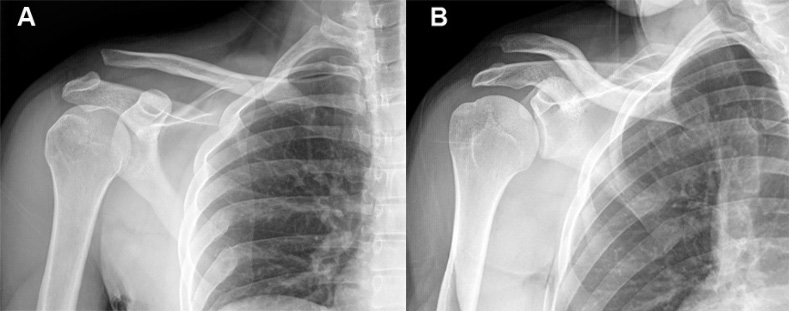
Figure 1. Pre-surgical X-rays of the right shoulder showing type V acromioclavicular dislocation (Rockwood classification). A) Zanca view. B) True anteroposterior view.
Source: Own elaboration.
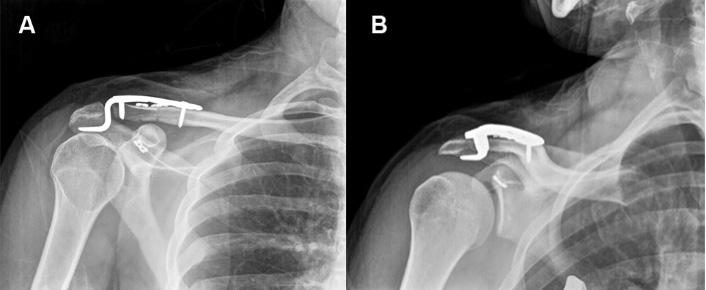
Immediate postoperative X-rays of the right shoulder showing the anatomical reduction of the acromioclavicular dislocation using the modified double-fixation open reduction technique. A) Zanca view.
B) True anteroposterior view.
Source: Own elaboration.
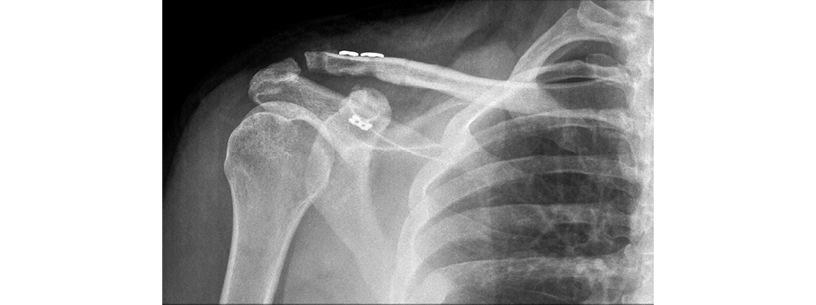
X-ray (Zanca view) of the right shoulder at the last follow-up, showing complete removal of the hook plate and fixation screws, as well as anatomical reduction of the preserved acromioclavicular joint without osteolysis or heterotopic ossification.
Source: Own elaboration.
Discussion
The surgical technique for the treatment of acute AC dislocations used in the present study involves the reconstruction of the CC ligament using FiberTape™ and Dog Bone™ buttons and neutralizing the construct with an AC HP. In this study, which included a group of adult patients with AC dislocations (type IV and V in the Rockwood classification) treated with this technique who were followed up for at least one year, there were no new dislocations, scapular dyskinesia or post-surgical infections, the level of pain was very low or nil, and most patients presented minimal osteolysis.
Several systematic reviews and meta-analyses have compared surgical treatment options for acute high-grade AC dislocations in the Rockwood classification.14-22 However, it has not been possible to establish which is the best treatment, as the evidence is not conclusive in terms of clinical outcomes.14-22 Most surgical procedures for AC dislocations mainly involve joint reduction and fixation, and reconstruction of the CC ligament to achieve lasting stability of the AC joint, both vertically and horizontally.20,23 Furthermore, it has been described that adequately restoring native joint biomechanics with an anatomic or non-anatomic approach would ensure an adequate healing rate as well as long-term stability, which is reflected in high patient satisfaction due to the absence of pain.14
A biomechanical evaluation of AC fixation devices by McConnell et al.24 demonstrated that HP fixation is the closest to the anatomy and function of a native AC joint, as it emulates the distal motion of the clavicle without deforming.24 The results of open reduction of the AC joint and internal fixation with clavicular HP have also been compared with those obtained using different methods of loop suspensory fixation. For example, Arirachakaran et al,15 Qi et al.17 and Pan et al.16 compared it with the TightRope™ technique, while Wang et al18 compared it with the use of suture buttons. In those studies, the findings on the performance of the techniques in terms of functionality are similar; however, some of these favored loop suspensory fixation procedures over HP fixation, as patients operated with this technique had a higher level of pain.15,17,17,18,25 In addition, some studies argue that non-rigid dynamic stabilization of the joint between the coracoid process and clavicle using loop suspensory fixation with synthetic materials may have similar results to HP fixation in which secondary surgery to remove the plate is not necessary.15-18,23
On the other hand, anatomical reconstruction of the CC ligament with autograft or synthetic materials provides better restoration of the horizontal and vertical stability of the joint, as it recreates the force vectors of the conoid and trapezoid ligaments.19,20,23 However, without the stabilizing fixation on the AC joint, high loads on the reconstructed CC ligament may result in loss of joint position (15-43%), rupture, and increased risk of fracture (21.3%).14,19,21,23 Isolated CC fixation techniques may result in anterior displacement of the clavicle relative to the acromion, leading to permanent loss of reduction and, consequently, anterior subluxation of the clavicle.26,27
In a finite element analysis study conducted by Sumanont et al,28 the stability of the AC joint after isolated CC fixation using a Dog Bone™ button was evaluated and that technique was compared to CC fixation combined with AC joint repair. In that study, it was found that concomitant AC joint repair decreases the peak stress on the CC fixation device by distributing it toward the repaired AC and reducing deformation in all forces. Furthermore, it was concluded that in high-grade AC dislocations, a combination of CC fixation and AC joint repair provides outstanding stability in the vertical and horizontal planes and helps to achieve restoration similar to the native joint.28
The technique proposed in this study combines anatomical reconstruction of the CC ligament using FiberTape™ and Dog Bone™ buttons with AC joint stabilization and HP fixation to restore joint biomechanics. Proper healing is achieved by redistributing loads in between the CC sutures (FiberTape™ and Dog Bone™ buttons) and neutralizing them with a HP and performing early rehabilitation. The HP promotes healing and stability of the entire construct, preventing displacements and re-luxation, and, although the subacromial space pressure increases, pain is minimal when rehabilitation is prompt. Furthermore, even though it has been argued that the main drawback of using HP is the need for a second intervention for its removal, we agree with McConnell et al,24 who support the use of AC fixation with this device, since the aim of the procedure is to replicate the stiffness of the native AC joint.
Arismendi et al.10 first described this technique in 2013, which consisted of the use of two type GII™ anchors with a double-charged anchor (Orthocord™) at the base of the coracoid process in a delta configuration.10 Although the technique produced satisfactory results, the senior author realized that this configuration did not anatomically reconstruct the CC and trapezoid ligaments, so he modified the technique and opted for the use of FiberTape™ sutures and the Dog Bone™ button. The use of FiberTape™ sutures in CC ligament reconstruction provides strength comparable to that achieved in tendon repair,20 while Dog Bone™ buttons prevent heavy sutures, such as the FiberTape™ sutures, from fracturing the clavicle or coracoid apophysis by supporting such force.19,28
Chang et al.11 compared the radiological and clinical outcomes of HP fixation with CC suture augmentation and those of isolated HP fixation for the treatment of acute unstable AC dislocation. These authors identified that augmentation with CC suture produces better short-term functional outcomes, a low level of pain, as well as a lower occurrence of subacromial osteolysis (p=0.02) and complications.11 Our technique reinforces said construct with Dog Bone™ buttons to secure the FiberTape™ sutures and avoid direct contact with the bone, which reduces the risk of fractures.
The ideal restoration of AC congruence is one that is stable over time, has a low incidence of re-luxation and pain, and shows optimal functional performance. The rate of loss of reduction reported in studies of different surgical treatments ranges from 3% to 43%.14,16,18,21,23 Our radiological outcomes showed that the CCD and ACD improved significantly after at least one year following the procedure, indicating that a safe anatomical reduction was achieved. No re-luxation occurred during the observation period, demonstrating that the reduction remained stable. Furthermore, rigid fixation with HP allowed complete healing of the AC joint and ligament, as well as rapid rehabilitation.
In the present study of a retrospective cohort, patient-perceived function was assessed using the QuickDASH questionnaire and post-procedure pain with the VAS. In the literature, the use of different validated scales to determine functional evolution after open reduction surgeries of AC dislocations is reported, including the QuickDASH score.20,23 The analysis of the subjective results of the patients included in this study showed a significant change (p=0.003) in the pre-surgical (median: 35 points) and post-surgical (median: 13 points) QuickDASH score, which implies a significant improvement in the perceived functional capacity in the short term. With regard to pain, it is worth mentioning that a pre-surgical pain assessment was not performed because only acute dislocations were studied, in which the pain level is usually at its highest. In this sense, it is deduced that there was an important change in pain since a low level was found one year or more after surgery (median VAS: 1).
The limitations of this study are typical of a retrospective study, as they include data quality and selection bias. Furthermore, the study had only one arm, with no control group and, consequently, results were only contrasted with those reported in the literature. Moreover, because the follow-up was relatively short (median: 20 months), prospective studies with longer follow-up periods are needed. Finally, although the sample of this study was small, we consider that the results presented could be comparable with those of other case series in which different techniques are used.
Conclusion
Based on the results of this study, we conclude that the technique used, in which both rigid fixation of the AC joint with an HP and repair of the CC ligament with sutures and buttons are performed, provided reliable, safe and stable healing that allowed prompt functional recovery without requiring prolonged immobilization with a sling.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Mazzocca AD, Arciero RA, Bicos J. Evaluation and Treatment of Acromioclavicular Joint Injuries. Am J Sports Med. 2007;35(2):316-29. https://doi.org/d52gbq.
2.Nolte PC, Lacheta L, Dekker TJ, Elrick BP, Millett PJ. Optimal Management of Acromioclavicular Dislocation: Current Perspectives. Orthop Res Rev. 2020;12:27-44. https://doi.org/kt7n.
3.Phadke A, Bakti N, Bawale R, Singh B. Current concepts in management of ACJ injuries. J Clin Orthop Trauma. 2019;10(3):480-85. https://doi.org/kt7p.
4.Jeong JY, Chun YM. Treatment of acute high-grade acromioclavicular joint dislocation. Clin Shoulder Elb. 2020;23(3):159-65. https://doi.org/kt7q.
5.Cook JB, Krul KP. Challenges in Treating Acromioclavicular Separations. Journal of the American Academy of Orthopaedic Surgeons. 2018;26(19):669-77. https://doi.org/kt7r.
6.Cibulas A, Leyva A, Cibulas G, Foss M, Boron A, Dennison J, et al. Acute Shoulder Injury. Radiol Clin North Am. 2019;57(5):883-96. https://doi.org/kt7s.
7.Granville-Chapman J, Torrance E, Rashid A, Funk L. The Rockwood classification in acute acromioclavicular joint injury does not correlate with symptoms. J Orthop Surg (Hong Kong). 2018;26(2):2309499018777886. https://doi.org/gjpkf9.
8.North AS, Wilkinson T. Surgical reconstruction of the acromioclavicular joint: Can we identify the optimal approach?. Strategies Trauma Limb Reconstr. 2018;13(2):69-74. https://doi.org/kt7v.
9.Cisneros LN, Reiriz JS. Management of acute unstable acromioclavicular joint injuries. Eur J Orthop Surg Traumatol. 2016;26(8):817-30. https://doi.org/kt7x.
10.Arismendi A, Jaramillo JC, Duque M del P. Fijación doble para luxación acromioclavicular aguda: recuperación de la estabilidad horizontal de la clavícula como factor clave para la reducción anatómica. Rev Colomb Ortop Traumatol. 2013;27(2):89-96. https://doi.org/f2m9z9.
11.Chang HM, Hong CK, Su WR, Wang TH, Chang CW, Tai TW. Comparison of clavicular hook plate with and without coracoclavicular suture fixation for acute acromioclavicular joint dislocation. Acta Orthop Traumatol Turc. 2019;53(6):408-13. https://doi.org/kt72.
12.World Medical Association (WMA). WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Fortaleza: 64th WMA General Assembly; 2013.
13.Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993 [cited 2023 Sep 21]. Available from: https://bit.ly/31gu7do.
14.Gowd AK, Liu JN, Cabarcas BC, Cvetanovich GL, Garcia GH, Manderle BJ, et al. Current Concepts in the Operative Management of Acromioclavicular Dislocations: A Systematic Review and Meta-analysis of Operative Techniques. Am J Sports Med. 2019;47(11):2745-58. https://doi.org/gfcdw2.
15.Arirachakaran A, Boonard M, Piyapittayanun P, Kanchanatawan W, Chaijenkij K, Prommahachai A, et al. Post-operative outcomes and complications of suspensory loop fixation device versus hook plate in acute unstable acromioclavicular joint dislocation: a systematic review and meta-analysis. J Orthop Traumatol. 2017;18(4):293-304. https://doi.org/kt73.
16.Pan X, Lv RY, Lv MG, Zhang DG. TightRope vs Clavicular Hook Plate for Rockwood III–V Acromioclavicular Dislocations: A Meta-Analysis. Orthop Surg. 2020;12(4):1045-52. https://doi.org/grpd5b.
17.Qi W, Xu Y, Yan Z, Zhan J, Lin J, Pan X, et al. The Tight-Rope Technique versus Clavicular Hook Plate for Treatment of Acute Acromioclavicular Joint Dislocation: A Systematic Review and Meta-Analysis. J Invest Surg. 2021;34(1):20-29. https://doi.org/grpd5d.
18.Wang C, Meng JH, Zhang YW, Shi MM. Suture Button Versus Hook Plate for Acute Unstable Acromioclavicular Joint Dislocation: A Meta-analysis. Am J Sports Med. 2020;48(4):1023-30. https://doi.org/gqv3z9.
19.Li Q, Hsueh PL, Chen YF. Coracoclavicular ligament reconstruction: a systematic review and a biomechanical study of a triple endobutton technique. Medicine (Baltimore). 2014;93(28):e193. https://doi.org/kt74.
20.Jordan RW, Malik S, Bentick K, Saithna A. Acromioclavicular joint augmentation at the time of coracoclavicular ligament reconstruction fails to improve functional outcomes despite significantly improved horizontal stability. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3747-63. https://doi.org/kt75.
21.Pill SG, Rush L, Arvesen J, Shanley E, Thigpen CA, Glomset JL, et al. Systematic review of the treatment of acromioclavicular joint disruption comparing number of tunnels and graft type. J Shoulder Elbow Surg. 2020;29(7S):S92-S100. https://doi.org/kt76.
22.Malahias MA, Sarlikiotis T, Brilakis E, Gerogiannis D, Avramidis G, Antonogiannakis E. The clinical outcome of the ‘Surgilig’ technique for the reconstruction of acromioclavicular dislocations: A systematic review. J Orthop. 2019;18:126-31. https://doi.org/kt77.
23.Modi CS, Beazley J, Zywiel MG, Lawrence TM, Veillette CJH. Controversies relating to the management of acromioclavicular joint dislocations. Bone Joint J. 2013;95-B(12):1595-602. https://doi.org/kt78.
24.McConnell AJ, Yoo DJ, Zdero R, Schemitsch EH, McKee MD. Methods of Operative Fixation of the Acromio-Clavicular Joint: A Biomechanical Comparison. J Orthop Trauma. 2007;21(4):248-53. https://doi.org/csqxjp.
25.Arirachakaran A, Boonard M, Piyapittayanun P, Phiphobmongkol V, Chaijenkij K, Kongtharvonskul J. Comparison of surgical outcomes between fixation with hook plate and loop suspensory fixation for acute unstable acromioclavicular joint dislocation: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2016;26(6):565-74. https://doi.org/kt79.
26.Baker JE, Nicandri GT, Young DC, Owen JR, Wayne JS. A cadaveric study examining acromioclavicular joint congruity after different methods of coracoclavicular loop repair. J Shoulder Elbow Surg. 2003;12(6):595-98. https://doi.org/d992h7.
27.Jerosch J, Filler T, Peuker E, Greig M, Siewering U. Which stabilization technique corrects anatomy best in patients with AC-separation?. Knee Surg Sports Traumatol Arthrosc. 1999;7(6):365-72. https://doi.org/dpdd56.
28.Sumanont S, Nopamassiri S, Boonrod A, Apiwatanakul P, Boonrod A, Phornphutkul C. Acromioclavicular joint dislocation: a Dog Bone button fixation alone versus Dog Bone button fixation augmented with acromioclavicular repair—a finite element analysis study. Eur J Orthop Surg Traumatol. 2018;28(6):1095-101. https://doi.org/kt8c.
 Daniela Galeano2
Daniela Galeano2 Catalina Hurtado2
Catalina Hurtado2 Ana Milena Herrera3
Ana Milena Herrera3