case report
Aneurysmal bone cyst: diagnostic differences with telangiectatic osteosarcoma. A case report
Quiste óseo aneurismático: diferencias diagnósticas con el osteosarcoma telangiectásico. Reporte de caso
Solangel Rodriguez-Materon1 Pablo Arbeláez Echeverry2
Pablo Arbeláez Echeverry2
1 Medical University of South Carolina, Orthopaedic Surgery Department, Charleston, South Carolina, United States.
2 Hospital Universitario San Ignacio, Orthopedics and Traumatology Department, Bogotá D.C., Colombia.
Open access
Received: 31/05/2021
Accepted: 29/04/2022
Corresponding author: Solangel Rodriguez-
Materon. Email: solangelroma@hotmail.com.
How to cite: Rodriguez-Materon S, Arbeláez-
Echeverry P. Aneurysmal bone cyst: diagnostic differences with telangiectatic osteosarcoma. A case report. Rev Col Or Tra. 2023;37(1):e6. English. doi: https://doi.org/10.58814/01208845.6
Cómo citar: Rodriguez-Materon S, Arbeláez-
Echeverry P. [Quiste óseo aneurismático: diferencias diagnósticas con el osteosarcoma telangiectásico. Reporte de caso]. Rev Col Or Tra. 2023;37(1):e6. English. doi: https://doi.org/10.58814/01208845.6
Copyright: ©2023 Sociedad Colombiana de Cirugía Ortopédica y Traumatología. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction: Symptoms, signs, imaging and histological findings of aneurysmal bone cyst (ABC) and telangiectatic osteosarcoma (TO) are similar, which makes them one of the most difficult differential diagnoses.
Case presentation: A 19-year-old woman attended the emergency department of a quaternary care hospital in Bogotá, Colombia, due to pain in the left hip. A lytic lesion in the femur was identified and the patient was referred to the outpatient clinic. Three days later, the patient returned to the emergency department with left hip pain and functional disability. By means of x-ray and MRI, a transcervical fracture of the hip was identified at the site of the lytic lesion, so the presence of ABC or TO was suspected. The patient was taken to surgery and a frozen section biopsy was performed, confirming the diagnosis of ABC. Consequently, curettage and reaming of the lesion were undertaken, followed by reduction and fixation of the fracture using the DHS (dynamic hip screw) system and placement of bone grafting and bone cement. Four days after the procedure, the patient was discharged. A follow-up at eight months showed complete recovery of hip functionality and absence of pain.
Conclusion: In patients with a high suspicion of this type of bone lesions, it is important to perform a histopathological study to confirm the diagnosis of ABC or TO, and to establish an adequate and timely treatment, which will undoubtedly contribute to a better prognosis, particularly in terms of survival.
Keywords: Bone cysts, Aneurysmal; Osteosarcoma; Biopsy; Diagnosis (MeSH).
Resumen
Introducción: los síntomas, signos y hallazgos imagenológicos e histológicos del quiste óseo aneurismático (QOA) y el osteosarcoma telangiectásico (OT) son similares, por lo que constituyen uno de los diagnósticos diferenciales más difíciles de establecer.
Presentación del caso: mujer de 19 años que asistió al servicio de urgencias de un hospital de cuarto nivel de atención en Bogotá por dolor en la cadera izquierda, donde se identificó lesión lítica en el cuello del fémur y se remitió a consulta externa. Tres días después, la paciente regresó al servicio de urgencias por dolor en la cadera izquierda e incapacidad funcional. Mediante radiografía y resonancia magnética, se identificó fractura transcervical de la cadera en el lugar de la lesión lítica, por lo que se sospechó la presencia de QOA u OT. La paciente fue llevada a cirugía y se realizó biopsia por congelación, confirmando el diagnóstico de QOA; por lo tanto, se realizó curetaje y fresado de la lesión, reducción y fijación de la fractura con sistema DHS (dynamic hip screw), y aplicación de injerto y cemento óseo. Cuatro días después del procedimiento, la paciente fue dada de alta. En el seguimiento a los ocho meses, se evidenció recuperación completa de la funcionalidad de la cadera y ausencia de dolor.
Conclusión: en pacientes en los que hay una alta sospecha de este tipo de lesiones óseas, es importante realizar un estudio histopatológico para confirmar el diagnóstico de QOA u OT, e instaurar un tratamiento adecuado y oportuno, que sin duda contribuirá a un mejor pronóstico, particularmente en términos de supervivencia.
Palabras clave: Quistes óseos aneurismáticos; Osteosarcoma; Biopsia; Diagnóstico (DeCS).
Introduction
Aneurysmal bone cyst (ABC) is a benign and potentially locally aggressive bone lesion that is characterized by rapid growth and occurs most frequently during the first two decades of life; primary ABC accounts for approximately 70% of cases.1 Signs and symptoms of ABC may vary and are often diagnosed incidentally through imaging tests such as x-ray, computed tomography (CT scan), and magnetic resonance imaging (MRI). However, as in most tumor lesions, biopsy with histological assessment is the gold standard test for diagnosis.
On the other hand, telangiectatic osteosarcoma (TO) is a malignant destructive tumor that makes up less than 4% of all cases of osteosarcoma. Like ABC, TO usually occurs in children, adolescents, and young adults. In addition, symptoms, signs, and histologic and imaging features of TO are similar to ABC, but TO has different survival and metastasis rates than ABC.2
The following is a case report of a 19-year-old female patient who presented with a pathologic fracture over a left hip lytic lesion. An open biopsy was performed, and the diagnosis of ABC was confirmed, so curettage and reaming of the lesion were undertaken, as well as reduction and fixation of the fracture and placement of bone graft and bone cement as definitive treatment.
Case presentation
A 19-year-old woman went to the emergency department of a quaternary care hospital in Bogotá after having left hip pain for five months, which had worsened in the last month. After admission, a plain x-ray of the pelvis showed a lytic lesion in the left proximal femur without acute fractures, so it was decided to assess the patient during an outpatient visit. Three days later, the patient returned to the emergency department complaining of sudden pain and functional disability in the left hip after turning over in bed. On admission, the patient reported no constitutional symptoms, sensation of lump, urinary and/or defecation-related symptoms, or decreased appetite. On physical examination, the patient had pain, but her vital signs were within normal range. The left lower limb was in external rotation, shortened, and the patient described pain on attempted mobilization. No evidence of neurovascular deficit or palpable masses in the extremity was found.
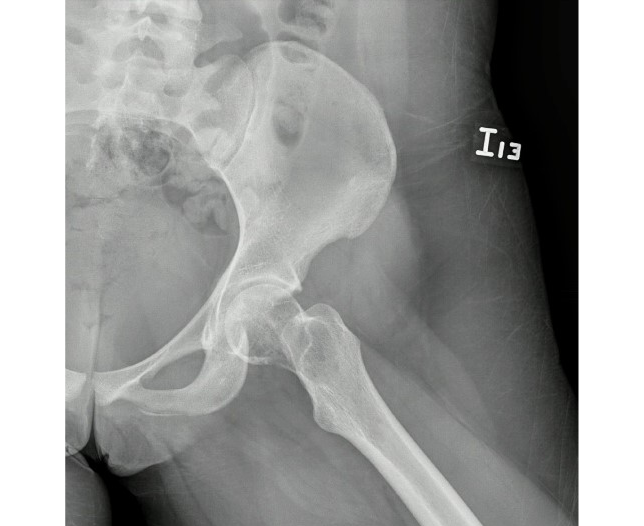
Laboratory tests on admission reported the following findings: blood count within normal limits, normal erythrocyte sedimentation rate, normal renal function tests (urea nitrogen and creatinine), normal alkaline phosphatase levels, normal parathyroid hormone level, slightly high levels of ionic calcium (1.8 mg/dL) and high levels of lactate dehydrogenase (836.33 u/L), as well as vitamin D3 deficiency (16 ng/mL). An x-ray of the pelvis and hip showed a pathological transcervical fracture of the left hip associated with the expansive lytic lesion initially found (Figures 1 and 2).
Figure 1. Antero-posterior x-ray of the pelvis showing a pathological transcervical fracture of the left hip associated with an expansive cystic lytic lesion, without periosteal reaction or adjacent soft tissue mass.
Source: Image obtained during the study.
Figure 2. X-ray of the left hip showing a pathological transcervical hip fracture associated with an expansive cystic lytic lesion, without periosteal reaction or adjacent soft tissue mass.
Source: Image obtained during the study.
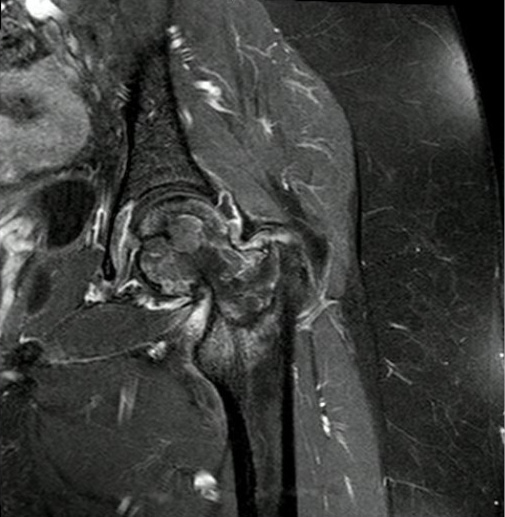
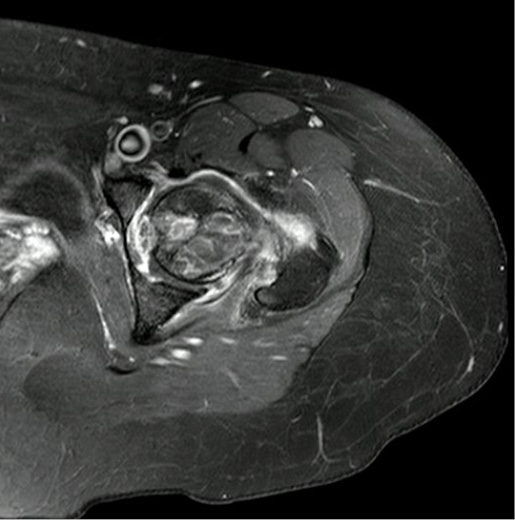
Subsequently, the patient was assessed by the orthopedic oncology service of the hospital, which ordered an MRI of the hip. This scan revealed an expansive lytic lesion with multiple fluid-fluid levels, thinning of the medial cortex of the femoral neck, and an associated pathological fracture (Figures 3 and 4). In view of these findings, the patient was taken to surgery in order to perform a frozen section biopsy and then establish the definitive treatment based on the pathology report, considering a second surgical procedure in case of malignancy.
Figure 3. Magnetic resonance imaging of the left hip. Coronal STIR sequence.
Source: Image obtained during the study.
Figure 4. Magnetic resonance imaging of the left hip. Axial STIR sequence.
Source: Image obtained during the study.
The frozen section biopsy performed during surgery revealed a histopathologic finding of ABC. Consequently, curettage and reaming of the lytic lesion, reduction and fixation of the fracture with a dynamic hip screw (DHS) system and an anti-rotation screw, and placement of bone graft and bone cement were performed during the same surgical procedure. At the end of surgery, a second specimen was taken for conducting a pathologic analysis of the margins of the lesion.
Along with the pain clinic service, the patient was given perioperative analgesia. Then, on the second postoperative day, physical therapy was started (mobilization and standing with crutches without weight bearing on the left lower limb), and on the fourth postoperative day the patient was discharged.
One week after discharge, a follow-up visit to the outpatient clinic took place. The patient did not report having any issues with pain management, and she was compliant with non-weight bearing instructions. In addition, the final pathology report was reviewed, which showed findings compatible with ABC, absence of malignancy, and benign critical value. The patient continued to attend physical rehabilitation sessions and clinical follow-up appointments. In the last follow-up appointment, performed 8 months after the fracture, the patient was asymptomatic and fully recovered in terms of functionality.
Discussion
For both general orthopedic surgeons and orthopedic oncologists, establishing the differences between TO and ABC is a diagnostic challenge. These two low-incidence diseases have very similar clinical, imaging and histopathological findings, and behavior, but their prognosis, treatment, morbidity, and mortality are quite different. With this in mind, early diagnosis and timely and accurate treatment are key to successful patient care and recovery.
Osteosarcoma is a major malignant bone tumor in children and adolescents, with TO being a rare variant that accounts for less than 4% of all osteosarcomas.2,3 Conversely, primary ABC is a benign bone lesion with an incidence ranging from 0.14 to 0.32 cases per 100 000 individuals.4 The age of onset for both tumors is between 10 and 20 years,1,2 and they usually affect males more than females, with a ratio of 2:12.5 and 1:1.2 for TO and ABC, respectively.1
In terms of location, ABC occurs mainly in the femur, tibia, fibula, humerus, skull, and posterior elements of the spine.1 TO is frequently located in the metaphysis of long bones, with the following distribution pattern: distal femur (42%), proximal tibia (17%), proximal humerus (9%), proximal femur (8%), followed by less frequent locations such as scapula, ribs, sternum, pelvis, skull bones, and mandible.2,5
The most common sign for both ABC and TO is the presence of edema or palpable mass,6 which are usually identified long after the onset of the disease. Besides edema, other signs and symptoms include pain and, sometimes, a pathologic fracture which appears as a complication at the site of the lesion.6,7
ABC appears as a lytic, hemorrhagic, circumscribed, cystic, expansive, radiolucent and locally aggressive lesion located within the metaphyseal area of a bone.8 Occasionally, the mass may elevate the periosteum, but typically, although eccentrically located, it remains contained by a thin layer of cortical bone. In very few cases, the mass is central or subperiosteal.8 On MRI, ABC exhibits fibrous septa and fluid-fluid levels, consistent with layers of solid blood within the cystic areas of the lesion.7 On the other hand, TO is characterized by purely lytic and expansive lesions, in some cases with minimal intralesional sclerosis. Most lesions are located in the metaphyseal area, but they may spread to the epiphysis in patients with closed epiphyseal plates.3 In addition, periosteal reaction and destruction of trabecular bone may sometimes be observed.7 On MRI, TO findings do not differ from those mentioned above for ABC.
Histologically, ABC is characterized by blood-filled cavities separated by thin, benign-looking fibrous septa and spindle cells.1,7 Furthermore, osteoid formation with or without osteoblastic rimming, inflammatory cells, and giant cells, such as osteoclasts, may be noted.6,7 For its part, TO exhibits blood-filled cavities with necrotic debris, separated by thick fibrous septa, in which atypical stromal cells, pleomorphism and, occasionally, osteoid matrix can be observed.3 It should be noted that 90% of the TO lesion is cystic before treatment.2
In light of the foregoing, there are many similar clinical, imaging and even histologic features between ABC and TO. Since one of these diseases is a malignant tumor, aggressive and timely treatment is a priority. The diagnosis of ABC or TO should be confirmed by histopathology before any definitive surgical procedure is undertaken. Needle biopsy is still controversial because the sample may not be sufficient to establish or confirm a diagnosis; for this reason, the indication is always to perform an open biopsy, as in the present case.
Extended curettage with embolization or en bloc resection plus placement of bone graft and/or bone graft substitute in patients with ABC has been reported to be an effective treatment.8 Likewise, the use of adjuvant sclerotherapy with cryotherapy or chemicals such as phenol has demonstrated a 10% to 20% reduction in disease recurrence.8
Patients with ABC have a favorable outcome, with an overall cure rate of 90-95%. It has also been reported that the most common complication in these patients is recurrence, which can occur up to two years after surgery.8 According to Maximen et al.1, in cases of recurrence or if the lesions cannot be excised, the use of denosumab may be considered as an additional treatment, taking into account the possibility of severe hypercalcemia as a side effect.
Regarding TO, initial treatment involves neoadjuvant chemotherapy (usually two to six sessions) using a minimum of two drugs. In addition, surgical excision of the lesion depends on its size, location, and the patient’s response to initial therapy. Adjuvant chemotherapy has been reported to be effective in cases of metastatic cancer, which spreads similarly to conventional osteosarcoma;2 however, patients with TO usually have a better response to treatment and a higher survival rate (up to 65% after five years) than those with conventional osteosarcoma.2 Prognosis in patients with TO is conditioned by chemosensitivity, the occurrence of necrosis, and the presence of metastases at the time of diagnosis.5
Conclusion
Due to the similarity of symptoms, signs, and radiologic and histologic findings, the diagnoses of ABC and TO may be mistaken for one another. Therefore, in cases of high suspicion of any of these bone lesions, histopathological study is critical to confirm the diagnosis and to establish an appropriate and timely treatment, which will undoubtedly contribute to a better prognosis, particularly in terms of survival. Open frozen section biopsy prior to any definitive surgical intervention is essential.
Informed consent
The patient’s informed consent (verbal authorization) was obtained for the preparation and publication of this case report.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Maximen J, Robin F, Tronchot A, Rossetti A, Ropars M, Guggenbuhl P. Denosumab in the management of Aneurysmal bone cyst. Joint Bone Spine. 2022;89(1):105260. https://doi.org/jvsf.
2.Limaiem F, Kuhn J, Khaddour K. Telangiectatic Osteosarcoma. Treasure Island: StatPearls Publishing; 2022.
3.Sangle NA, Layfield LJ. Telangiectatic osteosarcoma. Arch Pathol Lab Med. 2012;136(5):572-6. https://doi.org/gj25tw.
4.Oliveira AM, Perez-Atayde AR, Inwards CY, Medeiros F, Derr V, His BL, et al. USP6 and CDH11 oncogenes identify the neoplastic cell in primary aneurysmal bone cysts and are absent in so-called secondary aneurysmal bone cysts. Am J Pathol. 2004;165(5):1773-80. https://doi.org/brh6zw.
5.Jeyarani G, Jayaraman D, Menon G, Harshavardhaan JG, Rajendiran S, Murali A. Telangiectatic Osteosarcoma in a Young Child - A Case Report and Review of the Literature. J Orthop Case Rep. 2021;11(6):72-5. https://doi.org/jvsn.
6.WHO Classification of Tumours Editorial Board. Soft Tissue and Bone Tumors. 5th edition, Volume 3. WHO classification of tumours; 2020.
7.Rapp TB, Ward JP, Alaia MJ. Aneurysmal bone cyst. J Am Acad Orthop Surg. 2012;20(4):233-41. https://doi.org/f3ws6g.
8.Jalan D, Gupta A, Elhence A, Nalwa A, Bharti JN, Elhence P. Primary aneurysmal bone cyst of the calcaneum: A report of three cases and review of literature. Foot (Edinb). 2021;47:101795. https://doi.org/jvsq.
 Pablo Arbeláez Echeverry2
Pablo Arbeláez Echeverry2