original research
Outcomes in total knee replacement with and without a tourniquet: a cohort study
Desenlaces del reemplazo total de rodilla con y sin torniquete: un estudio de cohorte
Gabriel Narváez-Rodríguez1 José Reyes-Copello1
José Reyes-Copello1 Álvaro Reyes-Trujillo1
Álvaro Reyes-Trujillo1 Alfredo Castro-Dangond1
Alfredo Castro-Dangond1 Sofía Muñoz-Medina2
Sofía Muñoz-Medina2
1 Clínica Universitaria Colombia, Orthopedics Department, Bogotá D.C., Colombia.
2 Fundación Universitaria Sanitas, Research Unit, Bogotá D.C., Colombia.
Open access
Received: 03/04/2023
Accepted: 11/10/2023
Corresponding author: Gabriel Andrés Narváez Rodríguez. Departamento de Ortopedia, Clínica Universitaria Colombia. Bogotá D.C., Colombia. E-mail: gabonr-10@hotmail.com.
How to cite: Narváez-Rodríguez G, Reyes-Copello J, Reyes-Trujillo A, Castro-Dangond A, Muñoz-Medina S. Outcomes in total knee replacement with and without a tourniquet: a cohort study. Rev Col Or Tra. 2023;37(3):e28. English. doi: https://doi.org/10.58814/01208845.28
Cómo citar: Narváez-Rodríguez G, Reyes-Copello J, Reyes-Trujillo A, Castro-
Dangond A, Muñoz-Medina S. [Desenlaces del reemplazo total de rodilla con y sin torniquete: un estudio de cohorte]. Rev Col Or Tra. 2023;37(3):e28. English. doi:
https://doi.org/10.58814/01208845.28
Copyright: ©2023 Sociedad Colombiana de Cirugía Ortopédica y Traumatología. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction: Pneumatic tourniquet is commonly used during total knee replacement (TKR) surgery; however, this practice has been associated with complications derived from ischemia, making its use controversial.
Objective: To compare clinical and functional outcomes and frequency complications at 90 days in patients undergoing TKR with and without a tourniquet.
Methodology: Retrospective cohort study, including 393 patients with grade III and IV gonarthrosis who underwent primary TKR surgery with and without the use of a pneumatic tourniquet in two medical centers of Bogotá between 2014 and 2021, who were followed up for at least 90 days. Bivariate analyses (Student's t-tests, Mann-Whitney U and chi-square) were performed to establish differences between groups (with tourniquet versus without tourniquet).
Results: The median age was 67 years (interquartile range: 61-74 years) and 68.96% of the patients were women. A tourniquet was used in 45.80% and 2.54% presented some complication. Postoperative hematocrit loss (760mL vs. 679mL; p=0.13) and percentage of hemoglobin loss (17.8% vs. 17.1%; p=0.33) were higher in the TKR group in which no tourniquet was used. No statistically significant differences were found between groups in terms of pain, range of motion, duration of surgery, and presence of complications (p>0.05).
Conclusions: No significant differences were found between the use or non-use of tourniquet during TKR surgery in terms of pain, bleeding, range of motion, duration of surgery, and frequency of complications.
Keywords: Arthroplasty; Osteoarthritis; Osteoarthritis, Knee; Arthroplasty, Replacement, Knee; Tourniquets; Postoperative Complications (MeSH).
Resumen
Introducción. Durante la cirugía de reemplazo total de rodilla (RTR) se suele usar torniquete neumático; sin embargo, esta práctica se ha asociado a complicaciones derivadas de la isquemia, por lo que su uso es controversial.
Objetivo. Realizar una comparación entre la cirugía de RTR con torniquete y la cirugía de RTR sin torniquete en términos de desenlaces clínicos y funcionales, y frecuencia de complicaciones a 90 días.
Metodología. Estudio de cohorte retrospectivo realizado en 393 pacientes con gonartrosis grado III y IV sometidos a RTR primaria con o sin uso de torniquete neumático en dos centros médicos de Bogotá entre 2014 y 2021, en quienes se realizó seguimiento de mínimo 90 días. Se realizaron análisis bivariados (pruebas t de Student, U de Mann-Whitney y chi-cuadrado) para determinar diferencias entre grupos (con torniquete versus sin torniquete).
Resultados. La mediana de edad fue 67 años (rango intercuartílico: 61-74 años) y 68,96% de los pacientes eran mujeres. El torniquete se usó en 45,80% y 2,54% presentó alguna complicación. El grupo de RTR sin torniquete tuvo una mayor pérdida de hematocrito posoperatorio (760ml vs. 679ml; p=0,13) y porcentaje de pérdida de hemoglobina (17,8% versus 17,1%; p=0,33). No se encontraron diferencias estadísticamente significativas entre grupos en términos de dolor, rango de movilidad, duración de cirugía y presencia de complicaciones (p>0.05).
Conclusiones. No se observaron diferencias significativas entre haber o no haber usado torniquete durante la cirugía de RTR en términos de dolor, sangrado, rango de movilidad, duración de cirugía y frecuencia de complicaciones.
Palabras clave: Artroplastia; Osteoartrosis; Osteoartritis de la rodilla; Artroplastia de reemplazo de rodilla; Torniquetes; Complicaciones posoperatorias (DeCS).
Introduction
Total knee replacement (TKR) surgery is a procedure that is increasingly performed worldwide due to the high global prevalence of osteoarthrosis of the knee (654.1 million individuals in 2020).1 In this regard, it has been reported that about 675 000 TKRs are performed annually in the United States2 and 55 000 in Wales and England.3,4
The goal of primary TKR is to relieve pain, mechanically align the limb, and improve the quality of life in patients, and the percentage of good and excellent long-term outcomes exceeds 90% of cases.5 However, approximately 90% of TKRs are performed using a pneumatic tourniquet, as this reduces the technical difficulty of the procedure, allowing better visualization of the surgical field and reducing blood loss.6 Also, in cases in which cemented prostheses are used, TKR with pneumatic tourniquet improves the interdigitation of the cement on the bone, increasing the fixation of the components, which extends the useful life of the prosthesis.6
Although the use of the tourniquet has advantages during the surgical procedure, disadvantages have been described such as reduced range of motion, increased postoperative pain and the occurrence of venous thromboembolism and surgical site infections, as well as hypoxia, which alters the wound microenvironment.6,7 For example, deep vein thrombosis rates between 72% and 84% have been reported following TKR with tourniquet and its use has been associated with the development of venous insufficiency and calcified vessel damage.6,8 However, a systematic review including numerous clinical trials attempted to resolve the lack of consensus on the use of tourniquet during TKR. Although the results are heterogeneous, it is evident that a greater number of these trials recommend against its use due to the complications derived from ischemia.5
According to our literature search, the frequency of complications after the use of tourniquet during TKR has not been studied in Colombia, so having data on the Colombian population is a necessity. In view of the above, the aim of the study was to make a comparison between TKR surgery with tourniquet and TKR surgery without tourniquet in terms of clinical and functional outcomes and frequency of complications at 90 days.
Materials and methods
Study type, population, and sample
Retrospective cohort study conducted in adults with grade III and IV gonarthrosis undergoing primary TKR with and without pneumatic tourniquet between February 2014 and October 2021 in two medical centers specialized in joint replacements in Bogotá (Colombia), who were followed up postoperatively for at least 90 days (N=427). Patients who had implant-related problems (e.g., implant design errors, prosthesis ruptures and erosions, and insert rupture) and those who were taken to revision knee replacement surgery (n=34) were excluded.
Sample size was calculated taking into account a statistical power of 80%, a statistical significance level of 0.05, a ratio between the exposed and unexposed group of 1 to 1, a proportion of TKR complications between 11% and 22%,9,10 a delta of 0.11, and a probability of data loss of 10%, so the final sample size was 402 patients. Consecutive sampling of individuals meeting the above-mentioned characteristics was performed (n=393). Finally, it should be noted that, taking into account the percentage probability of data loss, it was decided to include more patients in whom a tourniquet was used than patients in whom it was not.
Variables
The medical record review allowed collecting data on the following variables: age, sex, weight, height, body mass index (BMI), presence of comorbidities, tourniquet use in TKR surgery, tourniquet use time, TKR laterality, outpatient management, hospitalization requirement, readmission requirement, postoperative visual analog scale (VAS) pain score (days 1, 3, 7 and 14), preoperative and postoperative knee range of motion (flexion and extension angles), duration of surgery, physical status, use of general anesthesia, change from regional to general anesthesia, type of surgery (navigated and non-navigated), occurrence of complications, type of complication, time elapsed from surgery to occurrence of complication, preoperative functionality, and blood loss.
It is worth mentioning that functionality in the operated limb was measured using the Oxford Knee Score questionnaire and the Western Ontario and McMaster Universities Arthritis Index (WOMAC) preoperatively. Physical status was also assessed using the American Society of Anesthesiologists (ASA) classification. In addition, to assess blood loss, the preoperative and postoperative blood count was reviewed, which was performed 6 hours after surgery or the following day. Thus, pre- and postoperative hemoglobin level, postoperative hemoglobin loss (in grams per deciliter [gr/dL]), postoperative hemoglobin loss percentage, pre- and postoperative hematocrit level, postoperative hematocrit loss (in milliliters [mL]), and postoperative hematocrit loss percentage were recorded. Hemoglobin loss (preoperative hemoglobin - postoperative hemoglobin x 100 / preoperative hemoglobin) and percentage of hemoglobin loss (weight x 60/100) were calculated using the formulas described by Bourke & Smith.11
Statistical analysis
Data are described using absolute and relative frequencies for categorical variables and measures of central tendency (means and medians) and dispersion (standard deviations and interquartile ranges [IQR]) for quantitative variables according to the distribution of the data (Kolmogorov-Smirnov test). Furthermore, the cumulative incidence of complications between groups (with tourniquet vs. without tourniquet) was calculated with a 95% confidence interval (CI), and a bivariate analysis was performed to determine the differences between groups in the variables considered using Student’s t-tests or Mann-Whitney U tests for quantitative variables and the chi-square test for categorical variables. A statistical significance level of p<0.05 was considered. All analyses were performed in the STATA software (Version 15).
Ethical considerations
This study followed the ethical principles for the conduct of biomedical research involving human subjects established in the Declaration of Helsinki12 and the technical, administrative and health research standards of Resolution 8430 of 1993, issued by the Colombian Ministry of Health.13 The study was also approved by the Research Ethics Committee of the Fundación Universitaria Sanitas (CEIFUS) by means of Minutes 011-22 of March 22, 2022.
Results
Of the 393 patients included in this study, 68.96% (n=271) were women and the median age was 67 years (IQR=61-74 years). Moreover, 44.27% had an ASA 2 physical status. Tourniquet was used during TKR in 45.80% (n=180) of the participants and 89.31% (n=351) received outpatient management (Table 1).
Table 1. Clinical characteristics of the patients included in the study (n=393).
|
Variable
|
n (%)
|
|
Sex
|
|
Male
|
122 (31.04)
|
|
Female
|
271 (68.96)
|
|
Age (in years) - median (IQR)
|
67 (61-74)
|
|
Weight - median (IQR)
|
71 (63-80)
|
|
Height - median (IQR)
|
1.6 (1.53-1.65)
|
|
BMI - median (IQR)
|
28.1 (25-30.9)
|
|
Comorbidities
|
|
High blood pressure
|
186 (47.33)
|
|
Hypothyroidism
|
85 (21.63)
|
|
Diabetes
|
39 (9.92)
|
|
Insulin dependence
|
11 (2.80)
|
|
Rheumatoid arthritis
|
29 (7.38)
|
|
Cancer
|
14 (3.56)
|
|
Chronic kidney disease
|
6 (1.53)
|
|
Cardiac diseases
|
6 (1.53)
|
|
Respiratory diseases (COPD, asthma, OSAHS, etc.)
|
27 (6.87)
|
|
ASA physical status classification
|
|
I
|
36 (9.16)
|
|
II
|
174 (44.27)
|
|
III
|
42 (10.68)
|
|
No data
|
141 (35.88)
|
|
Laterality of surgery
|
|
Right
|
197 (50.13)
|
|
Left
|
196 (49.87)
|
|
Outpatient management
|
|
Yes
|
351 (89.31)
|
|
No
|
42 (10.68)
|
|
Use of tourniquet
|
|
Yes
|
180 (45.80)
|
|
No
|
213 (54.20)
|
|
Preoperative Oxford Knee Score - median (IQR)
|
10 (7-15)
|
|
Preoperative WOMAC Osteoarthritis Index - median (IQR)
|
68 (24-80)
|
|
Range of motion of the operated knee - median (IQR)
|
|
Preoperative extension angle
|
0 (0-8)
|
|
Preoperative flexion angle
|
114.5 (104-124)
|
|
Postoperative extension angle
|
0
|
|
Postoperative flexion angle
|
108 (100-114)
|
|
General anesthesia
|
|
|
Yes
|
34 (8.65)
|
|
No
|
359 (91.35)
|
|
Switch from regional to general anesthesia
|
|
Bupivacaine – fentanyl
|
14 (3.86)
|
|
Tourniquet usage time - median (IQR)
|
49 (43-59)
|
|
Duration of the procedure (in minutes) - median (IQR)
|
67 (60-75)
|
|
Hemoglobin level (in mL) - median (IQR)
|
|
Preoperative
|
14.85 (14.1-15.8)
|
|
Postoperative
|
12.1 (11..4-13..15)
|
|
Hemoglobin loss (in g/dL) - median (IQR)
|
2.6 (1.9-3.3)
|
|
Percentage of hemoglobin loss - mean (SD)
|
17.4 (6..47)
|
|
Hematocrit level (in mL) - median (IQR)
|
|
Preoperative
|
44.6 (42.4-47)
|
|
Postoperative
|
37 (34..6-39..7)
|
|
Percentage of hematocrit loss - median (IQR)
|
7.25 (5.3-9.5)
|
|
Loss of hematocrit (in mL) - median (IQR)
|
723 (524-932)
|
|
Type of surgery
|
|
Navigated
|
56 (14.32)
|
|
Non-navigated
|
335 (85.68)
|
|
Complications
|
|
Yes
|
10 (2.54)
|
|
No
|
383 (97.46)
|
|
Type of complication
|
|
|
Wound dehiscence
|
2 (0.51)
|
|
Superficial infection of the operative site
|
1 (0.26)
|
|
Wound drainage
|
2 (0.51)
|
|
Gastrointestinal symptoms
|
2 (0.51)
|
|
Bleeding
|
1 (0.26)
|
|
Blister around wound
|
1 (0.26)
|
|
Popliteal artery injury
|
1 (0.26)
|
|
Readmission requirement
|
2 (0.51)
|
|
Hospitalization requirement
|
2 (0.51)
|
|
Time elapsed between surgery and the onset of the complication (in days) - mean (SD)
|
16.2 (13.10)
|
|
Visual Analog Pain Scale - median (IQR)
|
|
Postoperative day 1
|
1 (0-3)
|
|
Postoperative day 3
|
4 (2-6)
|
|
Postoperative day 7
|
4 (2-6)
|
|
Postoperative day 14
|
4 (2-4)
|
ASA: American Society of Anesthesiologists. SD: standard deviation. COPD: chronic obstructive pulmonary disease. BMI: body mass index. IQR: interquartile range. OSAHS: obstructive sleep apnea and hypopnea syndrome.. WOMAC: Western Ontario and McMaster Universities.
Source: Own elaboration.
Compared to the group in which a tourniquet was used, patients in the TKR group without tourniquet were younger in age (medians: 68 vs. 67 years; p=0.047), had a higher WOMAC osteoarthritis index (medians: 49 vs. 73; p=0.000), and required a switch from regional to general anesthesia more frequently (4 vs. 10 patients; p=0.024). In contrast, in the group of TKR with tourniquet there was a higher frequency of type II physical status in the ASA classification (103 vs. 71 patients; p=0.023) and of navigated surgery (40 vs. 16 procedures; p=0.000).
Regarding the range of mobility of the operated knee, a statistically significant difference was only observed between groups in the median preoperative extension angle (without tourniquet: 3° vs. with tourniquet: 0°; p=0.028). Although no statistically significant differences were found in the median flexion angle (preoperative: p=0.19; postoperative: p=0.56), the preoperative result was higher in the group without tourniquet. Regarding postoperative pain VAS score, the median was the same in both groups at days 1, 3 and 7; however, at day 14 it was lower in patients in whom tourniquet was used, but the difference was not statistically significant (p=0.12) (Table 2).
On the other hand, the duration of surgery was two minutes longer in the group without tourniquet (66 vs. 68 minutes). Furthermore, the presence of complications in patients taken to TKR without tourniquet was 3.7% (95%CI: 1.6%-7.2%), while in the TKR group with tourniquet it was 1.1% (95%CI: 0.1%-3.9%), a difference that was not statistically significant (p>0.05). Both the cumulative incidence of readmissions and hospitalizations in the TKR group without tourniquet was 0.94% (95%CI: 0.1%-3.3%) and 0 in the TKR group, and the difference was not statistically significant (p>0.05) (Table 2).
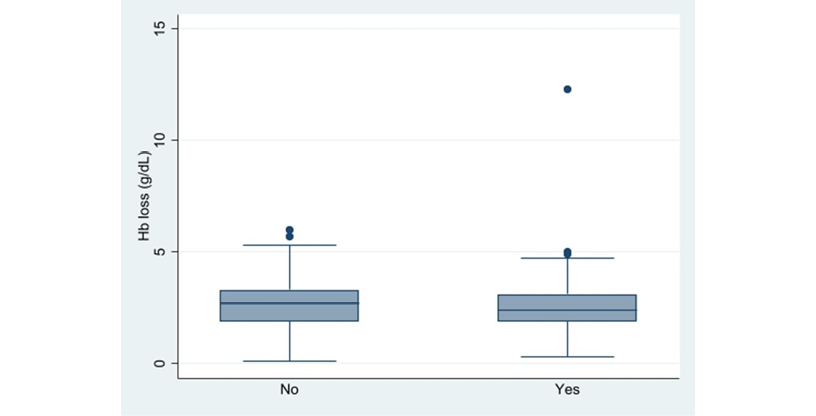
When hemoglobin was compared preoperatively and postoperatively, a median difference of 2.6 mL was found in the TKR group with tourniquet (p=0.000) and 2.8 mL in the group without tourniquet (p=0.000). Likewise, significant differences were observed between pre- and postoperative hematocrit levels in both groups (TKR with tourniquet: 7%; p=0.000. TKR without tourniquet: 7.8%; p=0.000). Conversely, no statistically significant differences were found between groups in terms of postoperative hemoglobin loss (p=0.19) (Figure 1) and percentage of postoperative hematocrit loss (p=0.17) (Figure 2). Finally, it was found that hemoglobin loss was similar in both groups (Table 2). Only one patient required blood transfusion, which was secondary to a vascular lesion of the popliteal artery during the surgical procedure that, in turn, led to hypovolemic shock.
Table 2. Comparison of patient characteristics depending on tourniquet use during total knee replacement surgery.
|
Variable
|
Tourniquet
(n= 180)
n (%)
|
No Tourniquet
(n=213)
n (%)
|
p-value
|
|
Sex
|
|
Male
|
56 (31.11)
|
66 (30.98)
|
0.98
|
|
Female
|
124 (68.88)
|
147 (69.01)
|
|
Age (in years) - median (IQR)
|
68 (61.5-76)
|
67 (61-73)
|
0.047
|
|
Weight - median (IQR)
|
70 (63-79)
|
72 (63-80)
|
0.32
|
|
Height - median (IQR)
|
1.59 (1.53-1.65)
|
1.6 (1.54-1.65)
|
0.4
|
|
BMI - median (IQR)
|
28.15 (25-30.35)
|
28.1 (25-31.2)
|
0.68
|
|
Comorbidities
|
|
High blood pressure
|
84 (46.66)
|
102 (47889)
|
0.81
|
|
Hypothyroidism
|
39 (21.66)
|
46 (21.59)
|
0.99
|
|
Diabetes
|
22 (12.22)
|
17 (7.98)
|
0.1
|
|
Insulin dependence
|
5 (2.77)
|
6 (2.81)
|
0.98
|
|
Rheumatoid arthritis
|
13 (7.22)
|
16 (7.51)
|
0.91
|
|
Cancer
|
5 (2.77)
|
9 (4.22)
|
0.44
|
|
Chronic kidney disease
|
1 (0.55)
|
5 (2.34)
|
0.15
|
|
Cardiac diseases
|
2 (1.11)
|
4 (1.87)
|
0.54
|
|
Respiratory diseases (COPD, asthma, OSAHS, etc.)
|
8 (4.44)
|
19 (8.92)
|
0.08
|
|
ASA physical status classification
|
|
I
|
20 (11.11)
|
16 (7.51)
|
0.023
|
|
II
|
103 (57.22)
|
71(33.33)
|
|
III
|
15 (8.33)
|
27 (12.67)
|
|
Laterality of surgery
|
|
Right
|
90 (50)
|
106 (49.76)
|
0.96
|
|
Left
|
90 (50)
|
107 (50.23)
|
|
Outpatient management
|
|
Yes
|
156 (86.66)
|
190 (89.20)
|
0.54
|
|
No
|
21 (11.66)
|
21 (9.86)
|
|
Preoperative Oxford Knee Score - median (IQR)
|
11 (7-15)
|
10 (7-14)
|
0.54
|
|
Preoperative WOMAC Osteoarthritis Index - median (IQR)
|
49 (20-75)
|
73 (61-82)
|
0.000
|
|
Range of motion of the operated knee - median (IQR)
|
|
Preoperative extension angle
|
3 (0-8)
|
0 (0-5)
|
0.028
|
|
Preoperative flexion angle
|
112 (100-122)
|
116 (105-125)
|
0.19
|
|
Postoperative extension angle
|
0 (0-3)
|
0 (0-0)
|
0.18
|
|
Postoperative flexion angle
|
108 (100-114)
|
108 (100-115.5)
|
0.56
|
|
General anesthesia
|
|
|
|
|
Yes
|
20 (11.11)
|
14 (6.57)
|
0.11
|
|
No
|
160 (88.88)
|
199 (93.42)
|
359 (91.35)
|
|
Switch from regional to general anesthesia
|
4 (2.22)
|
10 (4.69)
|
0.024
|
|
Duration of the procedure (in minutes) - median (IQR)
|
66 (59-78)
|
68 (61-74)
|
0.23
|
|
Hemoglobin level (in mL) - median (IQR)
|
|
Preoperative
|
14.8 (14-15.7)
|
14.9 (14.1-15.9)
|
0.33
|
|
Postoperative
|
12.2 (1.4-13.2)
|
12.1 11.4-13)
|
0.66
|
|
Hemoglobin loss (in g/dL) - median (IQR)
|
2.4 (1.9-3.1)
|
2.7 (1.7 -3.3)
|
0.19
|
|
Percentage of hemoglobin loss - mean (SD)
|
17.1 (0.5)
|
17.8 (0.5)
|
0.33
|
|
Hematocrit level (in mL) - median (IQR)
|
|
Preoperative
|
44.5 (42.5-46.8)
|
44.7 (42.1-47)
|
0.9
|
|
Postoperative
|
37.5 (34.8-40.2)
|
36.9 (34.4-39.6)
|
0.23
|
|
Percentage of hematocrit loss - median (IQR)
|
6.9 (5.3-9)
|
7.4 (5.3-9.9)
|
0.17
|
|
Postoperative hematocrit loss (in mL) - median (IQR)
|
679.5 (510-896)
|
760 (557-968)
|
0.13
|
|
Type of surgery
|
|
Navigated
|
40 (22.22)
|
16 (7.51)
|
0.000
|
|
Non-navigated
|
139 (77.22)
|
196 (92.02)
|
|
Complications
|
2 (1.11)
|
8 (3.75)
|
0.097
|
|
Type of complication
|
|
Wound dehiscence
|
1 (0.55)
|
1 (0.47)
|
0.62
|
|
Superficial infection of the operative site
|
1 (0.55)
|
0
|
|
Wound drainage
|
0
|
2 (0.94)
|
|
Gastrointestinal symptoms
|
0
|
2 (0.94)
|
|
Bleeding
|
0
|
1 (0.47)
|
|
Blister around wound
|
0
|
1 (0.47)
|
|
Popliteal artery injury
|
0
|
1 (0.47)
|
|
Hospitalization requirement
|
0
|
2 (0.94)
|
0.19
|
|
Readmission requirement
|
0
|
2 (0.94)
|
0.19
|
|
Time elapsed between surgery and the onset of the complication (in days) - mean (SD)
|
27.5 (21.9)
|
13.37 (10.32)
|
0.19
|
|
Visual Analog Pain Scale - median (IQR)
|
|
Postoperative day 1
|
1 (0-3)
|
1 (0-3)
|
0.83
|
|
Postoperative day 3
|
4 (2-6)
|
4 (2-6)
|
0.06
|
|
Postoperative day 7
|
4 (2-6)
|
4 (2-6)
|
0.23
|
|
Postoperative day 14
|
3 (2-4)
|
4 (2-5)
|
0.12
|
ASA: American Society of Anesthesiologists. SD: standard deviation. COPD: chronic obstructive pulmonary disease. BMI: body mass index. IQR: interquartile range. OSAHS: obstructive sleep apnea and hypopnea syndrome.. WOMAC: Western Ontario and McMaster Universities.
Source: Own elaboration.
Figure 1. Hemoglobin loss in grams over deciliters among patients who underwent total knee replacement with tourniquet and without tourniquet.
Source: Own elaboration with STATA (Version 15).
Figure 2. Percentage of hematocrit loss among patients who underwent total knee replacement with tourniquet and without tourniquet.
Source: Own elaboration with STATA (Version 15).
Discussion
The occurrence of TKR complications ranges from 11% to 20.8%5 and the most common are surgical site infection, venous thromboembolism, neurovascular injury, periprosthetic fractures, extensor mechanism injury, and joint stiffness.4,5,14 In contrast, arterial complications after TKR are rare (0.03-0.5%) and include acute ischemia, popliteal artery thrombosis, and aneurysms.15 In this study, a low frequency of complications was found (2.54%), the most common being wound-related problems such as dehiscence, drainage and superficial infection of the operative site.
Regarding the use of tourniquet during TKR and its association with ischemia, questions have arisen as to the degree of wound and flap compromise by use.16 Accordingly, in a study conducted in the United Kingdom in 31 patients undergoing TKR who were divided into 3 groups according to tourniquet use (no tourniquet, tourniquet inflated at low pressure [125 mmhg above mean arterial pressure], and tourniquet inflated at high pressure [250 mmhg above mean arterial pressure]), it was reported that all groups presented different levels of critical hypoxia in the flaps, being higher in the high-pressure tourniquet group, so these authors recommend inflating the tourniquet to the lowest possible pressure when it has to be used, in order to minimize wound complications.16 In this study, the tourniquet pressure used was 120mmHg higher than the systolic pressure measured on admission to the operating room and there were no clinical signs of hypoxia in the wound flaps during follow-up.
It has been suggested not to use tourniquet in patients with peripheral vascular disease who present calcifications of the popliteal artery, as this may lead to the development of complications such as acute arterial occlusion, rupture of the blood vessel wall, aneurysms and atheroma detachment, which causes distal arterial occlusion.5 However, in a study conducted in Ireland in 40 patients taken to TKR, it was found that tourniquet use did not increase the risk of arterial injury in both patients with normal vasculature and those with mild peripheral arterial disease.17
In terms of postoperative functionality and knee range of motion, a meta-analysis reported that range of motion was 10.4° lower in patients in whom tourniquet was used during total knee arthroplasty in early stages of rehabilitation (≤10 days after surgery).18 In turn, the systematic review and meta-analysis by Alcelik et al.14 found that knee flexion within the first week was better in the no tourniquet group than in the tourniquet group (54°, 95%CI: 38°-88° vs. 70°, 95%CI: 45°-95°). According to these authors, this difference could be explained by the temporary loss of functionality in the compressed thigh muscles, as there was no difference in long-term knee flexion.14 In the present study, the median postoperative extension and flexion angles were 0° and 108°, respectively, and there were no statistically significant differences (p>0.05).
The risk of venous thromboembolism secondary to ischemia has been an area of debate, as tourniquetting may potentially increase the risk of deep venous thrombosis due to venous blood stasis in the lower extremity and may cause injury to calcified blood vessels.14 Furthermore, a meta-analysis reported that tourniquet use increases the risk of thromboembolic events (relative risk: 5; 95%CI: 1.31-19.10; p=0.02) and non-thrombotic complications (relative risk; 2.03, 95%CI: 1.12-3.67; p=0.02).18 However, no symptomatic thrombotic event occurred in this study.
On the other hand, in a randomized study carried out in Denmark in 70 patients who underwent total knee arthroplasty with and without tourniquet, who were followed up postoperatively at short (8 weeks) and long term (6 months and 1 year), it was found that the patients operated without tourniquet had better functional and clinical outcomes at 8 weeks in the Knee Injury and Osteoarthritis Outcome Score and the range of mobility of the knee. However, no significant differences in these variables were evident at long-term follow-up (p>0.05).19 In addition, in this research, postoperative pain and the use of analgesics were lower in patients without tourniquet, surgical time and visibility were similar in the groups, intraoperative blood loss was higher in the group operated without tourniquet, and postoperative blood transfusions were not required.19 In the present study, the TKR group without tourniquet had a mean blood loss 81 mL greater than those in whom tourniquet was used, but the difference was not statistically significant (p=0.13), and no differences were found between the groups in the VAS score at postoperative days 1, 3, 7 and 14 (mean: 4/10).
A meta-analysis and systematic literature review including 15 studies (991 patients) reported that there were no statistically significant differences between patients undergoing TKR with and without tourniquet in total (difference: 246.20mL, p=0.22) and postoperative blood loss measured at the drainage system (difference 18.93 mL; 95%CI: 124.24-86.38), transfusion rate (odds ratio=1.36; 95%CI: 0.58-3.19), and operative time (difference 8.30 minutes; 95%CI: 5.57-22.17, p=0.01).3 However, one of the studies included in this publication found a higher rate of intraoperative visibility problems in the TKR group without tourniquet (without tourniquet: 13/40 versus with tourniquet: 0/37).3 In another study, performed in 180 patients who received cemented total knee arthroplasty in Mexico, it was reported that the hemoglobin and operative bleeding differential was lower when a tourniquet was used (p=0.008) and the blood transfusion rate (32.8%) was not correlated with ischemia (p=0.301).20 In this study, only one patient required blood transfusion.
Concerning surgical time in TKR surgery, it has been reported that the use of tourniquet reduces this time by 5.01 minutes (95%CI: 8.31-1.70; p=0.003).21,22 However, Zhang et al.18 found in a meta-analysis that operative time was 4.57 minutes shorter in the group of individuals undergoing total knee arthroplasty without tourniquet (95% CI: 7.59-1.56; p<0.01). In the present study, operative time was 2 minutes longer in the TKR group without tourniquet, although the difference was not statistically significant (p=0.23).
Regarding hospital stay, a systematic literature review and meta-analysis including 41 studies (2819 patients) described that the average hospital stay was significantly shorter in the group of patients who underwent total knee arthroplasty without tourniquet (6.44±3.48 days) than in those who used a tourniquet (7.72±3.54 days) (95%CI: 0.69-1.15; p<0.001).20 As for the postoperative management of the patients included in this study, it was found that the procedure was done on an outpatient basis in 88% and 90% of the individuals in the groups with and without tourniquet, respectively.
To the best of our knowledge, this is the first cohort study conducted in the Colombian population that analyzes the use of tourniquet in TKR surgery, which is its main strength. On the other hand, the limitations of the research include the short follow-up time and its retrospective nature since the medical records may have incomplete data.
Conclusion
In this study, there were no statistically significant differences between TKR with and without tourniquet in terms of pain, range of motion, hemoglobin loss, duration of surgery, and development of complications in patients with grade III and IV gonarthrosis.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29-30:100587. https://doi.org/gmpbdx.
2.Bager CL, Karsdal M, Bihlet A, Thudium C, Byrjalsen I, Bay-Jensen AC. Incidence of total hip and total knee replacements from the prospective epidemiologic risk factor study: considerations for event driven clinical trial design. BMC Musculoskelet Disord. 2019;20(1):303. https://doi.org/kz5f.
3.Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. 2010;17(2):141-7. https://doi.org/dmqvbk.
4.Wall PDH, Ahmed I, Edwin C, Farhan-Alanie MM, Parsons H, Price AJ, et al. Tourniquet use in total knee replacement surgery: a feasibility study and pilot randomised controlled trial (SAFE-TKR study). BMJ Open. 2021;11(1):e043564. https://doi.org/kz5g.
5.Vivacqua T, Barroso M, Matos P, Pires e Albuquerque R, Cavanellas N, Barretto JM. The use of tourniquet during total knee replacement in patients with and without popliteal artery calcification. Rev Bras Ortop. 2018;53(2):165-70. https://doi.org/gq9jmm.
6.Gazendam A, Wood TJ. Cochrane in CORR®: Tourniquet Use For Knee Replacement Surgery. Clin Orthop Relat Res. 2021;479(3):445-51. https://doi.org/kz5h.
7.Kumar N, Yadav C, Singh S, Kumar A, Vaithlingam A, Yadav S. Evaluation of pain in bilateral total knee replacement with and without tourniquet; a prospective randomized control trial. J Clin Orthop Trauma. 2015;6(2):85-8. https://doi.org/kz5j.
8.Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1121-30. https://doi.org/dprr36.
9.Souza GDA, Ramalho RSC, Albuquerque RSPE, Barretto JM, Chaves RSM, de Sousa EB. Higher risk of complications after total knee arthroplasty in octogenarians. Acta Ortopédica Bras. 2020;28(4):177-81. https://doi.org/kz5k.
10.Nham FH, Patel I, Zalikha AK, El-Othmani MM. Epidemiology of primary and revision total knee arthroplasty: analysis of demographics, comorbidities and outcomes from the national inpatient sample. Arthroplasty. 2023;5(1):18. https://doi.org/kz5m.
11.Lopez-Picado A, Albinarrate A, Barrachina B. Determination of Perioperative Blood Loss: Accuracy or Approximation? Anesth Analg. 2017;125(1):280-6. https://doi.org/gbkjqr.
12.World Medical Association (WMA). WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Fortaleza: 64th WMA General Assembly; 2013.
13.Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993 [cited 2023 Oct 23]. Available from: https://bit.ly/31gu7do.
14.Alcelik I, Pollock RD, Sukeik M, Bettany-Saltikov J, Armstrong PM, Fismer P. A comparison of outcomes with and without a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Arthroplasty. marzo de 2012;27(3):331-40. https://doi.org/djvzd4.
15.Arthur JR, Spangehl MJ. Tourniquet Use in Total Knee Arthroplasty. J Knee Surg. 2019;32(8):719-29. https://doi.org/gqsvcw.
16.Clarke MT, Longstaff L, Edwards D, Rushton N. Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg Br. 2001;83(1):40-4. https://doi.org/cgzmbq.
17.Walls RJ, O’Malley J, O’Flanagan SJ, Kenny PJ, Leahy AL, Keogh P. Total knee replacement under tourniquet control: A prospective study of the peripheral arterial vasculature using colour-assisted duplex ultrasonography. Surgeon. 2015;13(6):303-7. https://doi.org/f8mgmt.
18.Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L. The effects of a tourniquet used in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2014;9(1):13. https://doi.org/gbftf2.
19.Ejaz A, Laursen AC, Kappel A, Laursen MB, Jakobsen T, Rasmussen S, et al. Faster recovery without the use of a tourniquet in total knee arthroplasty: A randomized study of 70 patients. Acta Orthop. 2014;85(4):422-6. https://doi.org/gb9tw5.
20.Gutiérrez-García JA, Sierra-Pérez M, García-Velazco RA, Salas-Mora CA, Cisneros-González VM. Artroplastía total cementada de rodilla: comparación entre el uso o no de isquemia en el resultado postoperatorio inmediato. Acta Ortop. Mex. 2016;30(1):7-12.
21.Ahmed I, Chawla A, Underwood M, Price AJ, Metcalfe A, Hutchinson CE, et al. Time to reconsider the routine use of tourniquets in total knee arthroplasty surgery: an abridged version of a Cochrane systematic review and meta-analysis. Bone Joint J. 2021;103-B(5):830-9. https://doi.org/gqsvdt.
22.Yi S, Tan J, Chen C, Chen H, Huang W. The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2014;134(10):1469-76. https://doi.org/f6h8gg.
 José Reyes-Copello1
José Reyes-Copello1 Álvaro Reyes-Trujillo1
Álvaro Reyes-Trujillo1 Alfredo Castro-Dangond1
Alfredo Castro-Dangond1 Sofía Muñoz-Medina2
Sofía Muñoz-Medina2