case report
Spinal tuberculosis in a child following infection
with SARS-CoV-2: a case report
Tuberculosis vertebral posterior a infección por SARS-CoV-2 en un niño:
reporte de caso
David Jiménez-Marín1 Álvaro Toro-Posada2
Álvaro Toro-Posada2 Sergio Andrés Arroyave-Rivera3
Sergio Andrés Arroyave-Rivera3 Juan José García-Gil3
Juan José García-Gil3
1 Universidad Pontificia Bolivariana, Faculty of Medicine, Medellín, Colombia.
2 Hospital Universitario San Vicente Fundación, Orthopedics Service, Medellín, Colombia.
3 Universidad de Antioquia, Faculty of Medicine, Medellín, Colombia.Open access
Received: 24/08/2022
Accepted: 14/03/2023
Corresponding author: David Jiménez Marín. Facultad de Medicina, Universidad Pontificia Bolivariana, Medellín, Colombia. Email: davidjimenezm44@gmail.com.
How to cite: Jiménez-Marín D, Toro-
Posada A, Arroyave-Rivera SA, García-Gil JJ. Spinal tuberculosis in a child following infection with SARS-CoV-2: a case report. Rev Col Or Tra. 2023;37(2):e24. English. doi: https://doi.org/10.58814/01208845.24
Cómo citar: Jiménez-Marín D, Toro-Posada A, Arroyave-Rivera SA, García-Gil JJ. [Tuberculosis vertebral posterior a infección por SARS-CoV-2 en un niño: reporte de caso]. Rev Col Or Tra. 2023;37(2):e24. English. doi: https://doi.org/10.58814/01208845.24
Copyright: ©2023 Sociedad Colombiana de Cirugía Ortopédica y Traumatología. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction: Osteoarticular tuberculosis in children is a rare condition that accounts for a small percentage of extrapulmonary Mycobacterium tuberculosis infections.
Case presentation: A 30-month-old boy with a history of COVID-19 was taken to the emergency department due to antalgic pain, inability to stand up straight, and severe pain in decubitus position. The patient had elevated acute phase reactants levels, and computed tomography and magnetic resonance imaging showed destruction of L3 with bone marrow loss, vertebral collapse, and fluid collection, as well as involvement of L4. An open biopsy showed fluid collection with secretion, negative bacterial cultures, and positive molecular test for Mycobacterium tuberculosis. One week after admission, antitubercular pharmacological treatment was started and the patient was immobilized with a thoracolumbosacral orthosis. In a new admission to the emergency department, surgical drainage was performed due to wound dehiscence, secretion, and low-grade fever. However, in a subsequent follow-up, spondylodiscitis was found at L3 and L4, as well as epidural abscesses. Finally, once the orthosis management was completed, during a last follow-up, it was observed that the patient had residual thoracolumbar kyphosis, but no signs of radicular or spinal cord involvement, or osteoarticular deficit.
Conclusion: Spinal tuberculosis is a rare condition in the pediatric population, so clinical suspicion in all children with typical symptoms of the disease is always important.
Keywords: Tuberculosis; Spinal Diseases; COVID-19; SARS-CoV-2; Abscess; Pediatrics (MeSH).
Resumen
Introducción. La tuberculosis osteoarticular en niños es una condición infrecuente que representa un pequeño porcentaje de las infecciones extrapulmonares por Mycobacterium tuberculosis.
Presentación del caso. Niño de 30 meses con antecedente de que COVID-19 que fue llevado al servicio de urgencias por dolor en la marcha, imposibilidad para la bipedestación y dolor severo en posición decúbito. El paciente tenía niveles de reactantes de fase aguda elevados y mediante tomografía computarizada y resonancia magnética nuclear se evidenció destrucción de L3 con pérdida de la médula ósea, colapso vertebral y colección de fluido, así como compromiso de L4. Posteriormente, en una biopsia abierta se encontró colección de fluido con secreción, con resultado negativo en cultivos de bacterias y resultado positivo en prueba molecular de detección de Mycobacterium tuberculosis. Una semana después del ingreso, se inició manejo farmacológico antituberculoso y se inmovilizó con ortesis toracolumbosacra. En un nuevo ingreso al servicio de urgencias, se realizó drenaje quirúrgico por dehiscencia de la herida, secreción y febrícula. Sin embargo, en un control posterior se encontró espondilodiscitis en L3 y L4, y abscesos epidurales. Finalmente, una vez terminado el manejo con ortesis, en un último control se observó que el paciente presentaba cifosis toracolumbar residual, pero no tenía signos de compromisos radicular o medular, ni de déficit osteoarticular.
Conclusión. La tuberculosis vertebral es una condición infrecuente en población pediátrica, por lo que es importante tener una sospecha clínica en todos los niños con síntomas típicos de la enfermedad.
Palabras clave: Tuberculosis; Enfermedades de la Columna Vertebral; COVID-19; SARS-CoV-2; Absceso; Pediatría (DeCS).
Introduction
Osteoarticular tuberculosis in children is a rare condition that accounts for 5-6% of all cases of extrapulmonary tuberculosis in this population.1,2 Bone involvement is more common in older children, especially during the second decade of life, except for spinal involvement (vertebral tuberculosis or Pott’s disease), which is more frequent in children under five years of age.2 The occurrence of spinal tuberculosis could be explained by the presence of pre-existing vascular anastomosis between the intervertebral disc and the vertebral endplate in younger children.3 Pediatric osteoarticular tuberculosis is frequently associated with conditions resulting from immunosuppression.4
The association between this disease and SARS-CoV-2 is still unclear. At the time of writing this case report, to the best of the author’s knowledge, no studies have reported an association between this disease and SARS-CoV-2 infection in the pediatric population. On the other hand, it has been reported that pediatric osteoarticular tuberculosis is usually mistaken for other conditions with similar presentation on clinical, radiological, and laboratory assessment.4
This article reports the case of a 30-month-old boy who developed spinal tuberculosis following SARS CoV-2 infection, suggesting a possible association between the development of this disease and the immunosuppression caused by the virus infection.
Case presentation
A 30-month-old boy was taken to the emergency department of a tertiary care hospital in Medellín (Colombia) due to a history of gait pain, inability to stand upright, and severe pain in the decubitus position during the two weeks prior to his admission to the emergency room. These symptoms predominated during the afternoon and were constant and progressive. During the initial assessment, the parents reported that the patient had not suffered from loss of appetite, weakness, weight loss, fever or a history of associated trauma, and that he developed symptoms after experiencing asymptomatic SARS-CoV-2 infection. In the physical examination on admission, it was evident that the patient was unable to stand upright and had functional limitation to perform active and passive left hip range of motion with flexion contraction of 40°.
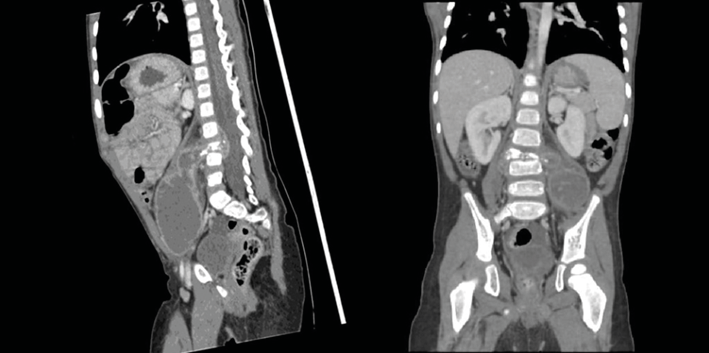
Considering the foregoing, the initial diagnostic suspicion was osteoarticular hip infection, for which an ultrasound, plain x-ray, acute phase reactant tests and hemoglobin analysis were performed, obtaining the following results: erythrocyte sedimentation rate of 120 mm/hour, C-reactive protein of 4.8 mg/dL (range: 0-1 mg/dL), hemoglobin of 10.5 g/dL, with no other cellular alterations or significant alterations in imaging tests. Due to the absence of significant imaging findings and mild elevation of acute phase reactant levels, a computed tomography (CT) scan of the abdomen and pelvis with contrast was performed to evaluate for the presence of psoas muscle abscess. The results of this study showed destruction of the L3 vertebral body with almost complete loss of bone marrow, as well as the presence of fluid collection in the adjacent soft tissues extending retroperitoneally (Figure 1).
Figure 1. Sagittal and coronal views of computed tomography of the abdomen and pelvis showing great destruction of the L3 vertebral body with secondary kyphoscoliosis and large fluid collection that protrudes into the spinal canal and the preperitoneal region, organized, with septa in its interior, and peripheral enhancement.
Source: Image obtained while conducting the study.
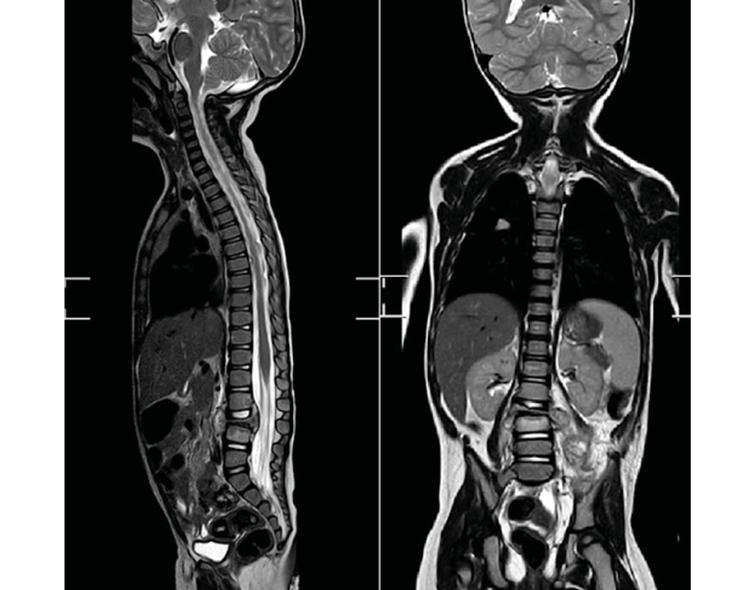
In view of the above, a simple whole spine MRI was performed, revealing extension of the abscess into the spinal canal, involvement of the upper endplate and the L4 vertebral body, and destruction of the underlying disc (Figure 2). Moreover, a chest X-ray was performed, showing bilateral interstitial opacities, as well as a spinal CT scan, showing right calcified perihilar lymph nodes. Based on these findings, chronic granulomatous disease was suspected, and an open biopsy was performed by the orthopedics service, during which samples were collected for bacterial cultures, identifying a collection of fluid with a yellowish-white, caseous, non-fetid secretion.
The result of the aerobic cultures and acid-fast bacilli test was negative; in addition, the Gram stain test was also negative for microorganisms. However, the patient tested positive in a molecular test for Mycobacterium tuberculosis. Therefore, spinal tuberculosis was diagnosed and, one week after admission, first phase antitubercular pharmacological treatment and immobilization with thoracolumbosacral orthosis was started.
On a new admission to the emergency room due to surgical wound dehiscence, secretion and low-grade fever, surgical drainage was performed; there was no evidence of pyogenic infection. However, a CT scan performed at a later follow-up identified spondylodiscitis at L3 and L4, with epidural abscesses draining into the skin through the surgical wound. Also, during this follow-up, the patient was in the fourth week of the first phase of antitubercular pharmacological treatment, with progressive improvement of symptoms and resumption of walking and standing upright. Once pharmacological treatment was completed, orthotic treatment was initiated. Finally, after completing treatment with orthosis, a last check-up showed that the patient had residual thoracolumbar kyphosis, but no signs of radicular or spinal cord involvement or osteoarticular deficit.
Figure 2. Sagittal and coronal view of the T1-weighted sequence MRI of the entire spine, showing destruction of the L3 vertebral body with loss of almost the entire vertebra and fluid collection extending to the preperitoneal area on both sides (especially the left), destruction of the underlying disc, and spinal canal without significant decrease in its amplitude.
Source: Image obtained while conducting the study.
Discussion
Spinal tuberculosis is the infection of one or more vertebral bodies by Mycobacterium tuberculosis, with or without spinal cord involvement,5,6 and is associated with conditions resulting from immunosuppression.4 In the case reported in this article, the possible predisposing condition that increased the risk of contracting spinal tuberculosis was SARS-CoV-2 infection, which occurred before the onset of musculoskeletal signs and symptoms. There is limited knowledge in the medical literature on the association between SARS-CoV-2 infection and tuberculosis, although there are studies reporting data on patients with coinfection or with COVID-19 and a history of tuberculosis.7,8 However, these studies are focused on adult population and bone involvement was only evidenced in one patient with disseminated tuberculosis.8
In terms of clinical features, there are important differences between the systemic symptoms of pulmonary and extrapulmonary involvement. In this regard, Devrim et al.,9 in a study of 128 patients under 14 years of age with active tuberculosis, found that 72% of children with extrapulmonary tuberculosis did not have fever, cough, malaise, or weight loss. This is consistent with the case reported, since only systemic involvement was evidenced in the follow-up with weight gain after the initiation of antitubercular pharmacological treatment.
The diagnosis of spinal tuberculosis in the pediatric population is complex, and in countries with a low incidence of tuberculosis, it is almost always late, due to the low index of suspicion.10 Unfortunately, in regions where this disease is endemic, diagnosis may be delayed due to poverty or limited access to medical care. On the other hand, it has been reported that 40-70% of patients present signs of spinal cord compression at the time of diagnosis.10
Currently, there are no treatment guidelines for spinal tuberculosis; however, it has been reported that between 82 and 98% of patients have a favorable response to antitubercular pharmacological treatment,11,12 so it remains the treatment of choice in the pediatric population.11 Some authors recommend performing surgery in patients with neurological deficits associated with spinal cord compression. However, a systematic review13 published in the Cochrane Database of Systematic Reviews in 2006, which compared surgical intervention plus chemotherapy with chemotherapy alone in patients with spinal tuberculosis, concluded that there is insufficient evidence to recommend routine surgery in the treatment of these patients since no statistically significant differences were found between the groups in terms of the outcomes studied (angle of kyphosis, reduction of neurological deficit, bone loss, absence of spinal tuberculosis, death, among others).
Conclusion
This article describes the case of a 30-month-old boy who presented with spinal tuberculosis following a SARS-CoV-2 infection. Spinal tuberculosis is a rare condition in the pediatric population, so it is important to have a clinical suspicion in all children with typical symptoms of the disease and not only in immunosuppressed patients, in order to be able to make an early diagnosis and provide timely treatment.
Informed consent
Informed consent was signed by the patient’s legal guardian. Furthermore, the case was approved by the Research Ethics Committee of the Fundación Hospitalaria San Vicente Paúl by means of Minutes 26, issued on September 10, 2021.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Tuli SM. General principles of osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;(398):11-19. https://doi.org/cwv88z.
2.Kritsaneepaiboon S, Andres MM, Tatco VR, Lim CCQ, Concepcion NDP. Extrapulmonary involvement in pediatric tuberculosis. Pediatr Radiol. 2017;47(10):1249-59. https://doi.org/gbv7pz.
3.Chunguang Z, Limin L, Rigao C, Yueming S, Hao L, Qingquan K, et al. Surgical treatment of kyphosis in children in healed stages of spinal tuberculosis. J Pediatr Orthop. 2010;30(3):271-6. https://doi.org/d3zjps.
4.Agarwal A. Paediatric osteoarticular tuberculosis: A review. J Clin Orthop Trauma. 2020;11(2):202-7. https://doi.org/kbdg.
5.Griffiths LI, Seddon H, Ball J, Darbyshire J, Wallace Fox, Kemp HBS, et al. Controlled trial of short-course regimens of chemotherapy in the ambulatory treatment of spinal tuberculosis. Results at three years of a study in Korea. Twelfth report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br. 1993;75(2):240-8. https://doi.org/gq6wx5.
6.Benzagmout M, Boujraf S, Chakour K, Chaoui Mel F. Pott’s disease in children. Surg Neurol Int. 2011;2:1. https://doi.org/fjzq8m.
7.Tadolini M, Codecasa LR, García-García JM, Blanc FX, Borisov S, Alffenaar JW, et al. Active tuberculosis, sequelae and COVID-19 co-infection: first cohort of 49 cases. Eur Respir J. 2020;56(1):2001398. https://doi.org/gmnjgs.
8.Stochino C, Villa S, Zucchi P, Parravicini P, Gori A, Raviglione MC. Clinical characteristics of COVID-19 and active tuberculosis co-infection in an Italian reference hospital. Eur Respir J. 2020;56(1):2001708. https://doi.org/gmnhpd.
9.Devrim I, Aktürk H, Bayram N, Apa H, Tulumoğlu S, Devrim F, et al. Differences between pediatric extra-pulmonary and pulmonary tuberculosis: a warning sign for the future. Mediterr J Hematol Infect Dis. 2014;6(1):e2014058. https://doi.org/kbds.
10.Arenas-Ruiz C, Díaz-Díaz A, Mesa-Monsalve JG, Trujillo M. Mal de Pott en un paciente pediátrico. Rev CES Med. 2014;28(2):253-62.
11.Agarwal A, Kant KS, Kumar A, Shaharyar A. One-year multidrug treatment for tuberculosis of the cervical spine in children. J Orthop Surg (Hong Kong). 2015;23(2):168-73. https://doi.org/f8nnw5.
12.Nene A, Bhojraj S. Results of nonsurgical treatment of thoracic spinal tuberculosis in adults. Spine J. 2005;5(1):79-84. https://doi.org/cnk89s.
13.Jutte PC, van Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev. 2006;(1):CD004532. https://doi.org/dtg2sg.
 Álvaro Toro-Posada2
Álvaro Toro-Posada2 Sergio Andrés Arroyave-Rivera3
Sergio Andrés Arroyave-Rivera3 Juan José García-Gil3
Juan José García-Gil3