Introduction
Acetabular fractures have an annual incidence of 3 cases per 100 000 people and represent a challenge for orthopedic surgeons.1,2 Anatomical congruence between the femoral head and the acetabulum is essential to obtain good long-term results in the treatment of this type of fracture, as it has been reported that displacements greater than 3mm can generate osteoarthrosis and poor functional outcomes in these patients.2 It has also been estimated that when osteosynthesis fails after surgery, the probability of having disabling osteoarthritis in the short term ranges between 30 and 40%, while the occurrence of bone structure displacement is about 5%.1-3 Moreover, it should be noted that the anatomy of the fracture may limit the use of regular implants and, consequently, these cases require hip arthroplasty using revision techniques for primary procedures.2
In the last decade, three-dimensional (3D) reconstruction of the human anatomy based on radiological studies has provided tools for planning surgeries, favoring the interpretation of reconstructions, as well as the determination of the surgical technique and implants required for the procedure.4,5 Thus, the use of 3D printing in preoperative planning allows for more effective diagnosis and simulation of the surgical procedure. In addition, the easy acquisition of materials and technology equipment, such as 3D printers and open-source software, has enabled orthopedists to obtain 3D biomodels from tomographic images.3
In view of the above, this case report describes the use of 3D printed biomodels in the preoperative planning of a total hip arthroplasty surgery for the treatment of a displaced acetabular fracture.
Case presentation
A 53-year-old man with no relevant medical history was admitted to the emergency department of a tertiary care public hospital in Lima (Peru) due to polytrauma to the chest and pelvis caused by a high-energy trauma sustained in a traffic accident. Physical examination of the patient revealed chest pain without respiratory distress and pain in the right hip. Imaging studies were also performed, but no bone injury was observed, so the patient was discharged 48 hours after admission to the emergency department.
Seven days after discharge, the patient presented moderate pain in the left hip and walking limitations, so he returned to the emergency department. Imaging studies were performed and a fracture of the left acetabulum involving the column was identified (Figure 1A-D), therefore, surgical treatment was indicated. However, the patient could only undergo surgery two months after being diagnosed due to a lack of financial resources and problems with his health insurance plan coverage. Surgery was developed in two stages: in the first stage, open reduction and internal fixation (ORIF) and filling with iliac crest graft were performed to maintain the bone stock, while the second stage consisted of a total hip arthroplasty (THA).
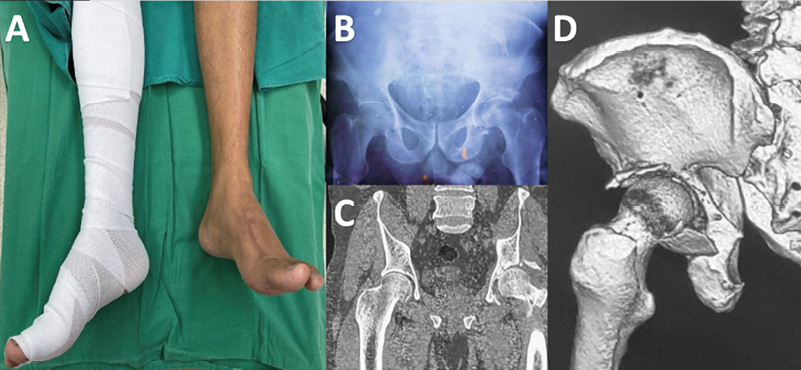
Figure 1. Clinical and imaging assessment of patient with acetabular fracture prior to surgery. A. Limited range of motion with predisposition to external rotation while flexing the affected hip. B. Anteroposterior x-ray of the pelvis. C and D. Computed tomography of the pelvis showing acetabular fracture.
Source: Images obtained while conducting the study.
Six months after surgery, the patient had very limited ambulation capacity and pain in the left hip that did not improve with conventional analgesics, so he resorted to the use of crutches and went to the emergency department. On physical examination, it was found that the leg was shortened by 3cm with respect to the other limb, with functional impairment, limited range of motion of the left hip and a tendency to external rotation when flexing the hip. With this in mind, an x-ray and a CT scan were performed, which showed severe deformation of the left acetabulum with posterosuperior migration of the femoral head, as well as necrosis of the femoral head in its entirety and posterosuperior bone defect of the acetabulum (Figure 2A-B), so the lesion was classified as a type IIIB acetabular defect according to the Paprosky classification.
Due to the acetabular defect and the complete loss of the left femoral head, it was decided to perform a THA. Preoperative planning was based on 3D biomodel printing, using the patient’s DICOM (Digital Imaging and Communications in Medicine) tomography files. These files were processed using the free and open-source software package 3D Slicer, in order to edit and select the anatomical area of the injury and to obtain three-dimensional object files in Standard Triangle Language (STL) format. Likewise, the free edition of Fusion 360 was used to design the 3D models of the prosthesis components (acetabular cup, liner, and femoral head and stem) (Figure 2C-E).
The STL files of the injury biomodels (pelvis and proximal femur) and the 3D components of the prosthesis allowed performing a digital preoperative planning, since they made possible the observation of the area of the bone defect and the determination of the sizes of the acetabular wedge and cup, as well as the femoral head graft, which were included in the treatment in order to support the remnants of the acetabular columns. These STL files were imported into the integrated 3D printer software (Creality CR-10 V2), and printing was performed using biodegradable resin material (polylactic acid), which took approximately 12 hours (Figure 2F-G).
3D biomodels of the prosthetic components and the pelvis showing the bone defect were used to simulate the THA technique and process, and based on this simulation, the most appropriate component layout and measurements (acetabular cup: 48mm; acetabular wedge: 50 x 10mm) were established (Figure 2C-E). Subsequently, the biomodels were sterilized with ethylene oxide for use during the surgery.
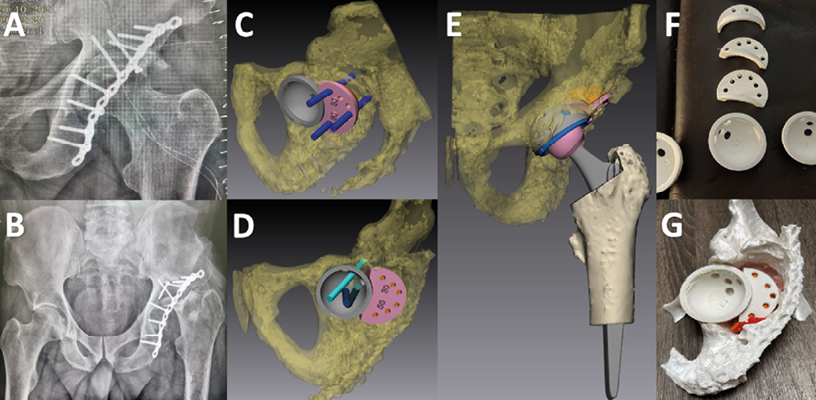
Figure 2. Postoperative imaging studies and preoperative planning using 3D. A. Anteroposterior x-ray of the pelvis performed in the immediate postoperative period. B. X-ray of the pelvis taken six months after the first surgery showing severe deformation of the left acetabulum with posterosuperior migration of the femoral head and necrosis of the femoral head. C-G. Design, printing, and preoperative planning using 3D bioprints that were used to determine the sizes of the acetabular cup (48mm) and the acetabular wedge (50mm x 30mm).
Source: Images obtained while conducting the study.
During surgery, with the patient in lateral decubitus position and using a standard posterolateral approach to the hip, the femoral neck was surgically identified, and a femoral osteotomy was performed in situ, allowing access to the bone defect. Part of the reconstruction plate used in the first surgery was also identified. All anatomical findings were consistent with the printed model, which guided the identification of the acetabulum. In order to size and shape the acetabulum to fit the acetabular cup shell, a high-speed drill was used, and the center of the hip was recognized, so acetabular drills were used sequentially with a progressive increase in size (2 mm to 47 mm) at the desired location. Moreover, in situ surgical tests of the acetabular wedge and cup were compared with the 3D biomodel and then, the definitive components of the prosthesis were inserted. Also, a cadaver femoral head graft was used to fill the spaces in the bone defect, and 3 screws (6.5mm) were inserted into the acetabular wedge and another 3 screws (6.5mm) into the acetabular cup to provide stability during integration of each of these components (Figure 3A-B).
Regarding the procedure performed in the femur, a 13 mm cementless femoral stem (Zimmer) was used, followed by implantation of a 28 mm ceramic femoral head and polyethylene insert. Finally, adequate range of motion, correct arthroplasty stability, and soft tissue tension were tested (Figure 3C-E).
The patient had an optimal postoperative recovery and was discharged 5 days after surgery. Two weeks after surgery, the patient started physical therapy sessions, achieving partial assisted ambulation at three weeks and unassisted ambulation at 12 weeks. During the follow-ups performed over the subsequent 12 months, the patient did not present any complications.
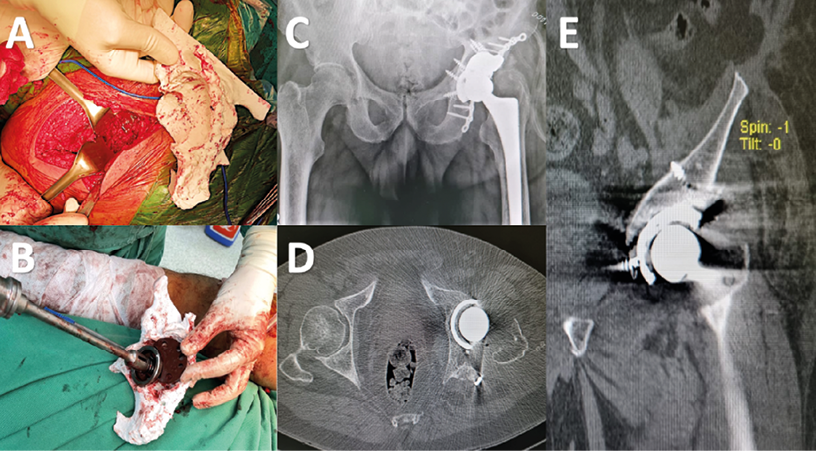
Figure 3. Final surgery and follow up with imaging studies. A-B. Acetabular surgery and placement of acetabular cup (48mm) and acetabular wedge (50mm x 30mm) with screws. C-E. Postoperative x-rays and CT scans showing proper open reduction plus internal fixation.
Source: Images obtained while conducting the study.
Discussion
Acetabular fractures are injuries usually resulting from high-energy traumas, such as traffic accidents or falls from heights, and about 75% of cases occur in young people. In this case report, such patterns partially concur with the patient’s situation since the cause of the fracture was a traffic accident and the patient was 53 years old.
The treatment of choice for acetabulum fractures is ORIF, which is recommended when there is fracture displacement greater than 2mm, fracture line in the load transfer zone, subluxation of the femoral head, and involvement of the anterior and posterior wall or column.4 In this regard, a systematic literature review that included 61 studies on acetabulum fractures in patients older than 55 years found that 55.42% (n=230) and 14.22% (n=59) of participants in 15 studies (n=415) reporting treatment data received ORIF and ORIF plus THA, respectively.1
On the other hand, performing THA as initial treatment is considered in patients with acetabulum fracture who present the following risk factors for failure of conventional treatment: femoral head impaction on the acetabulum, hip dislocation, femoral head damage, comminuted fracture, x-ray finding of impacted superior dome of the acetabulum (gull sign), or pre-existing osteoarthrosis. 5-7
Post-surgical complications in acetabulum fractures may result in alterations of the anatomy, pseudarthrosis, bone loss, implant failure, and avascular necrosis of the acetabulum or femur. Paprosky provided a classification of these bone defects based on their location and size.6 In the present case, the patient’s bone defect was classified as type IIIB because of acetabular wall involvement and superomedial femoral migration greater than 2cm.
The presence of complex bone defects in the acetabulum makes bone reconstruction difficult, thus requiring the implementation of strategies to treat this type of injury, including bone grafting, acetabular reconstruction using mesh, trabecular metal augmentation, or even customized prostheses.7 Strategy selection will depend on the surgeon’s expertise, the extent of the bone defect, financial resources, and available implants.7-9
In recent years, the development of 3D technologies has allowed the creation of new techniques to treat acetabular fractures, such as computer-assisted surgery. These new techniques have different application possibilities, including visualization and 3D printing of the injury and simulation of the surgical procedure on the printed models before and during surgery.
There are few case reports on the use of 3D biomodels for the treatment of acetabular fractures with bone defects. For example, Sánchez et al.8 described the case of a patient with complications related to acetabulum fracture, in whom the extent of the bone defect was assessed through 3D printing and the biomodel was used during surgery to determine the position of the implants. Similarly, Meesters et al.9 conducted a systematic review that included 19 studies on 3D biomodel-assisted acetabular fractures and found that the use of these models decreased operative time (162.5±79.0 minutes versus 296.4±56.0 minutes), blood loss (697.9±235.7mL versus 1097.2±415.5mL), use of fluoroscopy (9.3±5.9 times versus 22.5±20.4 times), and complications (OR: 0.5).9 Furthermore, Weng et al.10 used 3D printed models in the preoperative treatment planning of 23 patients with old acetabulum fractures, finding excellent, good and poor results in 14, 7 and 2 cases, respectively, as well as an operative time of 113.5 minutes, bleeding of 550.0 cc, and fluoroscopy use (12.7 shots on average).10 In our patient, 3D reconstruction was used for digital preoperative planning, determining the position and size of the implants. Also, a 3D printing of the lesion and the implants (acetabular cup and wedges) was produced and used in a simulation of the surgery and in the operating room to identify the anatomical structures and the appropriate size of the implants.
Regarding the disadvantages of using 3D biomodels in preoperative planning, it should be pointed out that certain technical requirements must be met, such as having a CT scan with good resolution (slice thickness no more than 0.1 mm). Printing time is another disadvantage, as each model takes an average of 10 to 24 hours to print, depending on its volume. In addition, it should be noted that, in the case of our patient, the presence of osteosynthesis material in the acetabulum produced artifacts in the imaging tests that generated a slight decrease in the accuracy of the 3D biomodel after its computerized segmentation.
Despite the above, using 3D biomodels in perioperative planning provides a full-scale representation of the lesion that offers a detailed view of the bone defect to the surgeon and makes it possible to identify the most appropriate areas to approach the injury. Moreover, the use of 3D biomodels allows for individualized operative planning for each patient in which the most suitable and capable implants are selected to withstand the mechanical resistance of the surgical reconstruction, reducing surgery time, bleeding and soft tissue damage.
Conclusions
Acetabular fractures are complex injuries, and their treatment represents a challenge for orthopedists, therefore, it is necessary to know the degree and extent of the injury to perform adequate preoperative planning and to select the appropriate implants. The use of 3D printed biomodels in preoperative planning for the treatment of complex acetabular injuries has led to good and satisfactory results in patients who meet these conditions.
Informed consent
By signing the informed consent form, the patient’s legal guardian authorized the use of the patient’s medical records for this case report.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged >55 years: a systematic review of the literature. Bone Joint J. 2014;96-B(2):157-63. https://doi.org/j8z9.
2.Boudissa M, Ruatti S, Kerschbaumer G, Milaire M, Merloz P, Tonetti J. Part 2: outcome of acetabular fractures and associated prognostic factors-a ten-year retrospective study of one hundred and fifty-six operated cases with open reduction and internal fixation. Int Orthop. 2016;40(10):2151-6. https://doi.org/j82b.
3.Rinne PP, Laitinen M K, Huttunen T, Kannus P, Mattila VM. The incidence and trauma mechanisms of acetabular fractures: A nationwide study in Finland between 1997 and 2014. Injury. 2017;48(10):2157-61. https://doi.org/gqtbqr.
4.Kelly J, Ladurner A, Rickman M. Surgical management of acetabular fractures - A contemporary literature review. Injury. 2020;51(10):2267-77. https://doi.org/gqtbqs.
5.Ortega-Briones A, Smith S, Rickman M. Acetabular Fractures in the Elderly: Midterm Outcomes of Column Stabilisation and Primary Arthroplasty. BioMed Res Int. 2017;4651518. https://doi.org/f9qx9c.
6.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9(1): 33-44. https://doi.org/ctv66k.
7.McCabe FJ, Kelly M, Farrell C, Abdelhalim M, Quinlan JF. Acetabular Lip Augmentation Devices for the Unstable Total Hip Replacement–A Systematic Review. Arthroplasty Today. 2021;12:1723. https://doi.org/j82c.
8.Sánchez-Pérez C, Rodríguez-Lozano G, Rojo-Manaute J, Vaquero-Martín J, & Chana-Rodríguez F. 3D surgical printing for preoperative planning of trabecular augments in acetabular fracture sequel. Injury. 2018;49(Suppl 2):S36–43. https://doi.org/j82d.
9.Meesters A, Trouwborst NM, de Vries J, Kraeima J, Witjes M, Doornberg JN, et al. Does 3D-Assisted Acetabular Fracture Surgery Improve Surgical Outcome and Physical Functioning? - A Systematic Review. J Pers Med. 2021;11(10):966. https://doi.org/j82f.
10.Wang XZ., Shi Z, Lu QL, Xie W, Chen L, Li XG, et al. [Treatment of old acetabular posterior wall fracture with 3D printing combined with composite plate internal fixation]. Zhongguo Gu Shang. 2019;32(5):395-400. https://doi.org/j82g.