Original article
Stingray injuries in patients treated at a secondary care hospital in Colombia: a case series
Lesiones por picadura de raya en pacientes atendidos en un hospital de segundo nivel en Colombia: serie de casos
Lorena García-Agudelo1 Mónica Liseth Holguín-Barrera1
Mónica Liseth Holguín-Barrera1 Gelber Yesid Barrera-Diaz2
Gelber Yesid Barrera-Diaz2 Jeinny Lucero Ruiz-Muñoz2
Jeinny Lucero Ruiz-Muñoz2
1 Hospital Regional de la Orinoquía, Research Office, Yopal, Colombia.
2 Universidad de Boyacá, Faculty of Health Sciences, Tunja, Colombia.
Open access
Received: 25/07/2022
Accepted: 09/01/2023
Corresponding author: Jeinny Lucero Ruiz Muñoz. Oficina de Investigación, Hospital Regional de la Orinoquía, Yopal, Colombia. Email: jeinnyruizm@gmail.com.
How to cite: García-Agudelo L, Holguín-
Barrera ML, Barrera-Diaz GY, Ruiz-Muñoz JL. Stingray injuries in patients treated at a secondary care level hospital in Colombia: a case series. Rev Col Or Tra. 2023;37(2):e12. English. doi: https://doi.org/10.58814/01208845.12
Cómo citar: García-Agudelo L, Holguín-
Barrera ML, Barrera-Diaz GY, Ruiz-Muñoz JL. [Lesiones por picadura de raya en pacientes atendidos en un hospital de segundo nivel en Colombia: serie de casos]. Rev Col Or Tra. 2023;37(2):e12. English. doi: https://doi.org/10.58814/01208845.12
Copyright: ©2023 Sociedad Colombiana de Cirugía Ortopédica y Traumatología. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, as long as the original author and source are credited.
Abstract
Introduction: Stingray injuries are the most common cause of fish stings and can be caused by marine and freshwater stingrays.
Objective: To characterize patients treated at a secondary care hospital in Colombia between 2019 and 2021 due to freshwater stingray injuries.
Methodology: Retrospective case series in which 10 patients were included. Data were obtained from hospital medical records and are described using absolute frequencies and percentages for qualitative variables and means and standard deviations for quantitative variables. Sociodemographic and clinical variables were taken into account.
Results: All participants were male, with a mean age of 43.5 years (standard deviation: ±20.74), and 50% were from rural areas. Feet (50%) were the anatomical region most affected by these injuries, followed by the hindfoot (25%), and the leg (25%). 70% of the patients presented complications (compartment syndrome [1 case], cellulitis [4 cases] and abscess [2 cases]). All participants received antibiotic therapy and surgical debridement, the average length of hospital stay was 16.2 days, and no deaths were reported.
Conclusion: Stingray sting is an injury of interest to the health area that requires an adequate and timely therapeutic approach to avoid complications and sequelae.
Keywords: Skates, Fish; Animals Poisonous; Wound infection; Abscess (MeSH).
Resumen
Introducción. Las lesiones por raya son la afectación más común de picaduras de peces y pueden ser causadas por rayas marinas y de agua dulce.
Objetivo. Caracterizar a los pacientes atendidos en un hospital de segundo nivel en Colombia entre 2019 y 2021 por lesiones por picadura de raya de agua dulce.
Metodología. Serie de casos retrospectiva en la que se incluyeron 10 pacientes. Los datos fueron obtenidos de las historias clínicas del hospital y se describen utilizando frecuencias absolutas y porcentajes para las variables cualitativas, y medias y desviaciones estándar para las cuantitativas. Se tuvieron en cuenta variables sociodemográficas y clínicas.
Resultados. Todos los participantes eran hombres, el promedio de edad fue 43,5 años (desviación estándar: ±20,74) y el 50% provenía de zonas rurales. Los pies (50%) fueron la región anatómica más afectada por estas lesiones, seguidos por el cuello del pie (25%) y la pierna (25%). El 70% de los pacientes presentó complicaciones (síndrome compartimental [1 caso], celulitis [4 casos] y absceso [2 casos]). Todos los participantes recibieron antibioticoterapia y desbridamiento quirúrgico, el promedio de duración de la estancia hospitalaria fue 16,2 días y no se reportaron muertes.
Conclusión. La picadura por raya es una lesión de interés en el área de la salud que requiere de un abordaje terapéutico adecuado y oportuno para evitar complicaciones y secuelas.
Palabras clave: Raya, Pez; Animales venenosos; Infección de heridas; Absceso (DeCS).
Introduction
Stingray injuries are the most common cause of fish bites worldwide and can be caused by saltwater stingrays or freshwater stingrays. Freshwater stingrays (family Potamotrygonidae) inhabit lakes and river systems in South America, Africa, Laos and Vietnam. Injuries caused by the latter type of stingrays are common in the Brazilian Amazon, accounting for 88.4% of the aquatic animal injuries reported in that region.1,2 Moreover, fishers have been identified as the most exposed population.3
Stingrays are dorsoventrally flattened, diamond-shaped fish with strong pectoral fins; they also have one to three saw-edged teeth (2.5 to >30cm long) at the base of the tail.1,4 A stingray bite results in trauma and toxicity since the action of its venom is necrotizing, edematous, proteolytic, neurotoxic, and myotoxic. This produces local signs and symptoms, mainly pain associated with local edema, which can lead to complications such as ulcers, tetanus, necrosis, and associated bacterial infection.2,3
Treatment of stingray bites includes modulation of pain and implementation of measures to prevent associated infections and necrosis by debriding the wound and administering antibiotic therapy in a timely manner.4
Considering the above, the objective of this research was to characterize patients treated at a secondary care hospital in Colombia between 2019 and 2021 due to freshwater stingray injuries.
Methodology
Study type, population and sample
Retrospective case series including patients treated at a secondary care hospital in Colombia for lower limb wounds or injuries due to freshwater stingray bites between 2019 and 2021. Patients with injuries due to causes other than stingray bites were excluded.
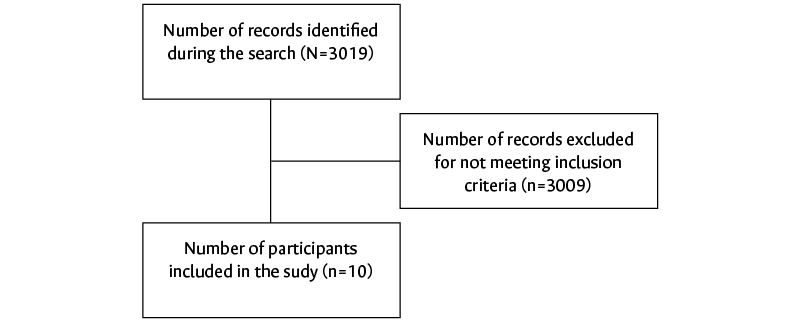
The medical records of patients with lower extremity injuries were reviewed, filtering by the following International Classification of Diseases (ICD) 10 codes: S711, S717, S718, S810, S817, S818, S819, S822, S861, S910, S911, S912, S913, S917, S968, T131, and T135. A total of 3 019 patient records with a diagnosis of lower limb injuries or wounds were found, of which 3 009 people were excluded because their injuries or wounds were caused by other mechanisms. Consequently, only 10 participants met the required criteria and were therefore included in the study (Figure 1).
Figure 1. Participant search and selection flowchart.
Source: Own elaboration.
Variables
For each study participant, the following data were recorded: sociodemographic variables (age, sex, and place of origin) and clinical variables (anatomical area affected, time elapsed between the event and admission to the emergency department, signs and symptoms, signs of local infection [edema, flushing, and warmth], characteristics of the injury, diagnostic tests used, management and treatments administered [antibiotic therapy, surgery, advanced wound care, and/or plastic surgery], number of surgical procedures, wound culture results, length of hospital stay, complications, and outcome).
Statistical analysis
Data collected from the medical records were entered into a database created in Microsoft Excel (version 2013). Data were described using absolute frequencies and percentages for qualitative variables and means and standard deviations (SD) for quantitative variables. Moreover, 95% confidence intervals (CI) were calculated.
Ethical considerations
This research followed the ethical principles for conducting biomedical studies involving human subjects established in the Declaration of Helsinki5 and the scientific, technical and administrative standards for health research established in Resolution 8430 of 1993 issued by the Colombian Ministry of Health.6 In addition, the study was approved by the Health Research Ethics Committee of the hospital where the study was conducted through Minutes 012 of 2022.
Results
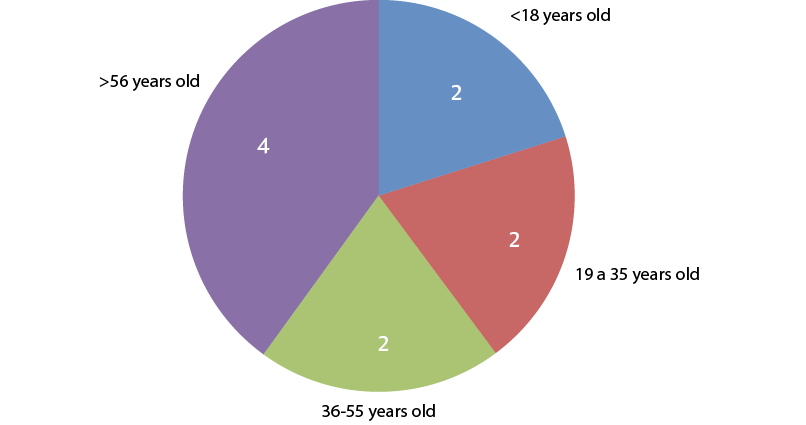
All patients were male, and the mean age was 43.5 years (SD±20.74) (95%CI: 30.64-56.35), with the minimum and maximum ages ranging from 17 to 66 years. Age distribution is presented in Figure 2. Furthermore, 50% of the patients were from rural areas.
Figure 2. Age distribution of the patients included in the study.
Source: Own elaboration.
With respect to the anatomical region where the injury occurred, the feet were the most frequently affected area with 50% of the bites (Figure 3 and 4), followed by the hindfoot, (Figure 5) and the leg (Figure 6), each with 25%.
Figure 3. Stingray injury in the forefoot.
Source: Own elaboration.
Figure 4. Stingray bite in the midfoot (dorsal side) of the right lower limb. The wound shows a coverage defect, sphacelate tissue, necrosis and granulation, tendon exposure, mild serous exudate, defined and adherent edges, perilesional skin with erythema, and mild edema.
Source: Own elaboration.
Figures 5A and B. Stingray injury on the lateral and medial aspect of the right leg, with coverage defect, sphacelate tissue, necrosis, granulation, and defined edges.
Source: Own elaboration.
Figures 6A and B. Stingray injury on the right side of the right leg, with coverage defect, granulation, defined edges and evidence of an adequate healing process.
Source: Own elaboration.
The time elapsed between the accident with the freshwater stingray and admission to the emergency department was less than 6 hours in 20% of the patients, between 7 and 24 hours in 10%, and more than 24 hours in 70%. Moreover, 66.66% (n=2) of the patients who attended the emergency department early, that is, within 24 hours after the event (n=3), had no complications and the average length of hospital stay was 7 days. In the context of this research, it should be noted that, due to the religious beliefs prevalent in the region, some people first go to ensalmadores (quacks) to perform the ensalme rite, which is a special prayer that seeks to cure and prevent the progression of the infection. For this reason, many patients seek medical attention late, only when the pain forces them to do so.
Regarding clinical manifestations, it was found that all patients presented severe pain. In addition, 80% (n=8) of the participants had signs of local infection (edema, flushing, and warmth), with half of them showing pus (n=4) and the other half showing necrosis (n=4). Moreover, 70% of the patients presented complications, namely compartment syndrome (1 case), cellulitis (4 cases), and abscess (2 cases).
Finally, the diagnostic tests performed were plain x-ray (90%), Doppler ultrasound (20%) and soft tissue ultrasonography (30%). The characteristics of the patients are summarized in Table 1.
Table 1. Clinical characteristics of the patients included in the study.
|
Patient
|
Antibiotic therapy
|
Number of surgical procedures
|
Wound culture
|
Advanced wound care treatment
|
Length of hospital stay in days
|
Complications
|
|
1
|
Meropenem
|
7
|
Aeromona hydrophila
|
Yes
|
43
|
Compartment syndrome
|
|
2
|
Oxacillin + Clindamycin
|
1
|
Negative
|
No
|
5
|
None
|
|
3
|
Ciprofloxacin + Clindamycin + Gentamicin
|
7
|
Negative
|
Yes
|
22
|
Cellulitis
|
|
4
|
Oxacillin + Clindamycin
|
2
|
Negative
|
No
|
7
|
None
|
|
5
|
Ciprofloxacin + Gentamicin
|
3
|
Edwarsiella tarda
|
No
|
18
|
Cellulitis
|
|
6
|
Meropenem
|
3
|
Escherichia coli
|
No
|
16
|
Abscess
|
|
7
|
Ciprofloxacin + Clindamycin
|
3
|
Negative
|
No
|
11
|
Cellulitis
|
|
8
|
Oxacillin + Gentamicin
|
2
|
Negative
|
No
|
8
|
None
|
|
9
|
Oxacillin + Gentamicin
|
3
|
Negative
|
No
|
18
|
Abscess
|
|
10
|
Oxacillin + Gentamicin
|
3
|
Negative
|
No
|
14
|
Cellulitis
|
Source: Own elaboration.
Regarding surgical management, wound lavage and debridement were performed in all patients, and the average number of interventions per patient was 3.4 (SD±2.01). Additionally, 70% of the participants presented coverage defect and 30% achieved wound closure and epithelialization. Likewise, 20% of the patients received advanced wound care treatment by a high-tech wound clinic and 60% of the participants required plastic surgery.
Finally, the average length of hospital stay was 16.2 days (SD±10.89; 95%CI: 9.45-22.94) and no patient required referral to a higher complexity hospital or died from the freshwater stingray injury.
Discussion
Stingrays are used for consumption and sport fishing and represent a source of income, so there are public health effects resulting from injuries caused by their bites.7 When the stingray is accidentally stepped on, it turns around, quickly moves its tail and stings the victim in a defensive action, causing a wound or laceration, making the lower limbs the most frequently affected anatomical area.4
It has been described that stingray poisoning causes intense pain and inflammation, as well as signs of local infection afterwards, with cellulitis and abscesses being the main complications, which coincides with the findings of the present study. In addition, their bite causes a laceration that allows bacteria such as Pseudomonas spp and Staphylococcus spp to enter the wound and, consequently, cause secondary infection.4,8 Wound complications are a medical concern, as the most serious risks include chronic ulcers, osteomyelitis, septicemia, ecthyma gangrenosum, tetanus, and necrotizing fasciitis.9
Stingray venom has effects on the cardiovascular, respiratory, nervous, and urinary systems. The most common signs and symptoms include fainting, weakness, nausea, anxiety, and sweating. In some cases, seizures, arrhythmias or cardiogenic shock may occur, although patients with cardiovascular changes usually return to normal within 24 hours.9
When dealing with stingray bites, it is necessary to wash the wound thoroughly, since this action can partially eliminate the venom. Afterwards, analgesics are administered to control pain; tetanus vaccine is administered since necrosis is a precondition for the proliferation of Clostridium tetani; and the injured area is subjected to heating at a temperature of approximately 45ºC for at least 30 minutes in order to denature the venom and, consequently, reduce pain. Elevating the affected limb also helps to reduce edema. When pain is severe, intravenous opioid analgesics or regional anesthesia may be administered. If there are deep wounds, complete surgical debridement under general anesthesia may be necessary. Thus, wounds should be left open and allowed to heal by secondary intention.8-11
The risk of infection is very high and is correlated with the size of the wound, so some authors suggest that antibiotic prophylaxis is unnecessary in patients with superficial wounds of less than 1 cm. In this sense, deep wounds or wounds with signs of envenomation should be explored and washed, and antibiotic prophylaxis should be initiated in the patient.11
One of the sequelae that may appear in patients who suffer stingray bites are coverage defects, which was evidenced in most of the cases included in this study. This outcome occurs because, usually, severe infections cause large soft tissue defects. Therefore, these patients require early coverage of the defect by the plastic surgery service depending on the individual characteristics of the case.12
In the present research, the most commonly used imaging study was plain x-ray; however, stingray barbs are not always radiopaque and may not be visible in this type of x-ray. For this reason, in cases of high suspicion of stingray bite, MRI is the most reliable diagnostic imaging tool.9
Regarding limitations, the fact that there is no ICD 10 coding for this type of injury and the retrospective design of this study did not allow for the identification of a representative number of patients despite the fact that it is known that a large number of people are admitted to this hospital for this type of injury.
Conclusion
Stingray bites are a significant injury in the field of health care; however, they have not been studied in depth, so their epidemiology is unknown. An adequate and timely therapeutic approach favors pain management and prevents complications and sequelae, so it is essential to follow up these patients until the wound has healed.
Conflicts of interest
None stated by the authors.
Funding
None stated by the authors.
Acknowledgments
None stated by the authors.
References
1.Rensch GP, Elston DM. Aquatic Antagonists: Stingray Injury Update. Cutis. 2019;103(3):138-40.
2.Gonçalves-Sachett JD, Vanderson-Souza S, Iran-Mendonça S, Shibuya A, Francesconi-Vale F, Peixoto-Costa F, et al. Delayed healthcare and secondary infections following freshwater stingray injuries: risk factors for a poorly understood health issue in the Amazon. Rev Soc Bras Med Trop. 2018;51(5):651-9. https://doi.org/gffxx3.
3.Blaizot R, Desrousseaux G, Joly MP, Vie A, Lu X, Senchyna A, et al. Pseudoaneurysm following a freshwater stingray injury. J Eur Acad Dermatol Venereol. 2019;33(10):e356-7. https://doi.org/j8fh.
4.Silva EO da, Filho EBG, Pardal PP de O, Ferreira S dos S, Diaz PRRR. Características de las lesiones de la raya de agua dulce (Potamotrygon sp.) en la isla de Marajó, Pará, Brasil (2017). Revista Eletrônica Acervo Saúde. 2018;11(3):e201. https://doi.org/j8gb.
5.World Medical Association (WMA). WMA Declaration of Helsinki – Ethical principles for medical research involving human subjects. Fortaleza: 64th WMA General Assembly; 2013.
6.Colombia. Ministerio de Salud. Resolución 8430 de 1993 (octubre 4): Por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud. Bogotá D.C.; octubre 4 de 1993 [cited 2023 May 02]. Available from: https://bit.ly/31gu7do.
7.Lasso CA, Morales-Betancourt MA, Garrone-Neto D, de Carvalho M (Eds.). Serie Editorial Recursos Hidrobiológicos y Pesqueros Continentales de Colombia. XV. Rayas de agua dulce (Potamotrygonidae) de Suramérica. Parte II: Colombia, Brasil, Perú, Bolivia, Paraguay, Uruguay y Argentina. Bogotá D.C.: Instituto de Investigación de Recursos Biológicos Alexander von Humboldt; 2016.
8.Martins-Abati PA, Quispe-Torrez PP, de Siqueira-França FO, Lambertini-Tozzi F, Bacelar-Guerreiro FM, Torres Dos Santos SA, et al. Injuries caused by freshwater stingrays in the Tapajós River Basin: a clinical and sociodemographic study. Rev Soc Bras Med Trop. 2018;50(3):374-8. https://doi.org/gbwqmb.
9.Haigh K, Delbridge P, Meda K, Chilamkurthi R. Stingray envenomation in a returning traveller: a complicated disease course. BMJ Case Rep. 2019;12(7): e228644. https://doi.org/j8k2.
10.Negreiros de Holanda M, Ferreira- Câmara O, da Silva DD, Bernade PS, Mota da Silva A, Malveira de Lima MV, et al. Accident and vascular injury with stingray in the Alto Juruá, Acre, Brazil: a case report. J Hum Growth Dev. 2019;29(3):427-32. https://doi.org/j8k3.
11.Luherne C, Luth T, Oehler E. Piqûre de raie pastenague: un cas en Polynésie française [Stingray injury: A case in French Polynesia]. Ann Dermatol Venereol. 2019;147(2):123-6. https://doi.org/d4622d.
12.Möllhoff N, Ehrl D, Giunta RE. Defektdeckung nach schweren Weichteilinfektionen: wann und wie? Chirurg. 2020;91(4):313-8. https://doi.org/j8k5.
 Mónica Liseth Holguín-Barrera1
Mónica Liseth Holguín-Barrera1 Gelber Yesid Barrera-Diaz2
Gelber Yesid Barrera-Diaz2 Jeinny Lucero Ruiz-Muñoz2
Jeinny Lucero Ruiz-Muñoz2