Introduction
Due to the increase in urban violence, gunshot wounds have become a major cause of morbidity and mortality, especially among young men. The incidence of penetrating spinal cord injuries due to firearm projectiles varies depending on the region, but it has been reported that the thoracic region is the most frequently involved area, followed by the lumbosacral and cervical regions.1-3
Some studies have established that the location of the lesion determines the occurrence of neurological deficit, with 70% of cervical lesions resulting in complete deficits and 70% of lesions in the lumbosacral region and cauda equina resulting in incomplete deficits. The main prognostic factor for recovery of patients with spinal cord injury is their initial neurological status, and the functional outcome is usually worse in patients with injuries caused by firearm projectiles. On the other hand, the follow-up period necessary to consider the functional status as definitive varies in the literature, ranging from 2 weeks to 6 months.1-5
Treatment of patients with gunshot wounds is based on advanced trauma life support (ATLS), administration of broad-spectrum intravenous antibiotics, and tetanus prophylaxis.1-12 Surgical management remains controversial and factors for its indication include the presence of cerebrospinal fluid fistula, progression of neurological deficit, and vertebral instability due to associated fractures. Currently, biomedical literature supports spinal decompression and projectile removal in patients with incomplete spinal cord injury. Moreover, other factors used to determine surgical treatment are the location of the projectile with evidence of migration (within the disc or spinal canal) and heavy metal toxicity in joints or within the disc.1,3-10,12-20
In this context, the following is the clinical case of a patient with a dual spinal cord injury caused by a firearm projectile lodged in the dural sac at the level of the cauda equina and incomplete neurological deficit, in whom the projectile was surgically removed.
A 21-year-old man was admitted to the emergency department of a tertiary care hospital in Bogotá (Colombia) due to multiple gunshot wounds (Figure 1), paraplegia, hypoesthesia in the lower limbs and saddle area, paresthesia in legs, and inability to move. Imaging studies identified the first entry orifice of the projectile in the right posterior thorax at the level of T5-T6, which caused pneumothorax; the second entry orifice in the right paravertebral region with fracture of L1 involving the pedicle and the right facet joint, with presence of small free bone fragments inside the medullary canal (Figure 2); and the third orifice in the midline spine at the level of S1-S2, with the projectile lodged in the dural sac and in contact with the cauda equina (Figure 3).
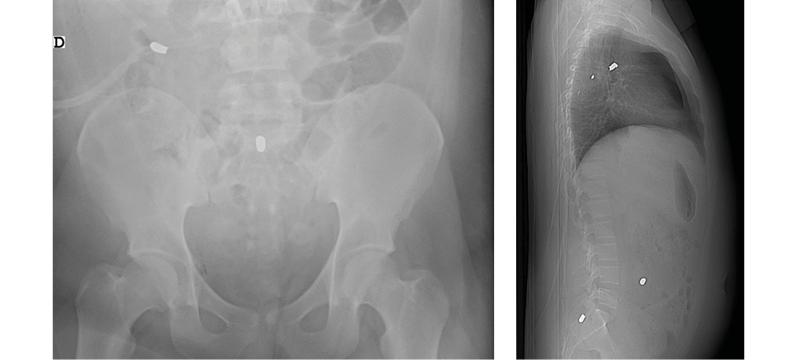
Figure 1. A): Anteroposterior pelvic radiograph. B) X-ray of the lateral spine showing multiple firearm projectiles.
Source: Image obtained while conducting the study.
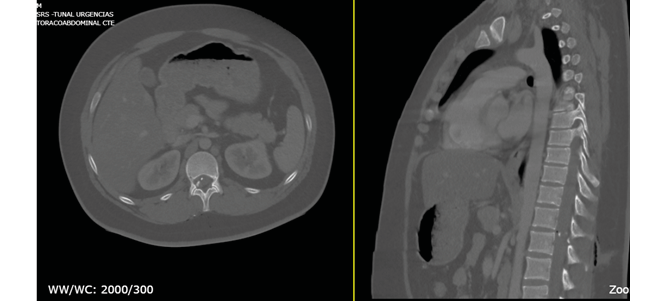
Figure 2. Computed tomography of thoracic spine showing L1 fracture and vertebral fragments within the spinal canal. A) Axial view. B) Sagittal view.
Source: Image obtained while conducting the study.

Figure 3. Computed tomography of the lumbosacral spine showing a projectile lodged in the vertebral canal at S1-S2. A) Axial view B) Sagittal view.
Source: Image obtained while conducting the study.
Three hours after admission, the general surgery service performed a thoracostomy and an exploratory laparotomy, finding a small lesion in the ascending colon without perforation, as well as the third projectile which was apparently in the abdominal wall and did not require removal. Nine hours after admission, the patient was assessed by the orthopedic spine service, finding no evidence of cerebrospinal fluid leakage. In addition, the assessment revealed strength in both lower limbs of 0/5 according to the Daniels muscle strength scale, areflexia, hypoesthesia in saddle area and lower limbs up to S1, and absence of cremasteric and bulbocavernosus reflex. Consequently, grade A spinal cord injury according to the American Spinal Injury Association Impairment Scale (ASIA) was determined between T12-L1.
Surgical procedure and postoperative evolution
In view of the foregoing, 12 hours after admission, the patient was taken to surgery to remove the projectile. The patient was positioned in prone position and a posterior approach was used in the lumbosacral midline. Dissection by anatomical planes until exposing the posterior arches of S1-S2 was performed, as well as laminectomy and longitudinal durotomy. However, the projectile could not be removed because it could not be located, so fluoroscopy was immediately performed, observing that the projectile had migrated cephalad to the L4-L5 intervertebral space (Figure 4), without evidence of projectile movement due to manipulation of the patient’s position, which included reverse Trendelenburg position. This was followed by laminectomy of L4-L5, exposure of the dural sac, and longitudinal durotomy. The projectile was located in the dural sac, anterior to the cauda equina, had no sharp edges, and floated freely in the cerebrospinal fluid, generating a bulging of the dural sac (Figure 5) that allowed predicting its location using a blunt dissector to avoid its cranial migration and achieve its removal. Finally, the projectile was extracted using a curved Kelly forceps and the roots of the cauda equina were found to be intact (Figures 3- 5). The dura was sutured, and the Valsalva maneuver was performed without evidence of cerebrospinal fluid leakage. Lastly, the wound was closed in the standard way.
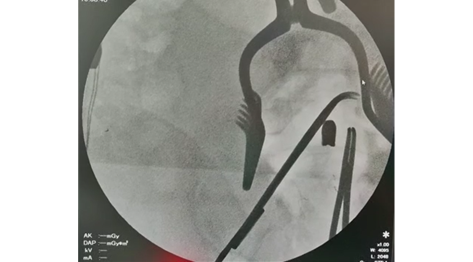
Figure 4. Fluoroscopy performed during surgery showing the location of the projectile at the level of L4-L5.
Source: Image obtained while conducting the study.
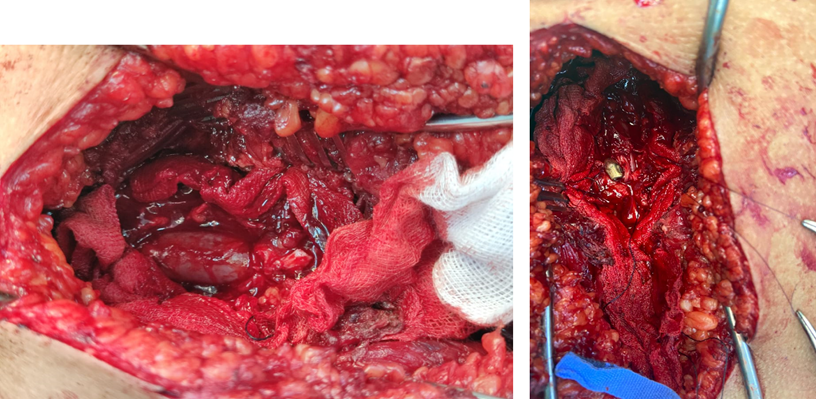
Figure 5. Surgical intervention performed to remove the projectile. A) Bulging of the dural sac. B) Projectile inside the dural sac at the level of L4-L5.
Source: Image obtained while conducting the study.
Fifteen days after the surgery, the patient presented dehiscence of the abdominal and lumbosacral wound and infection of the operative site, so the general surgery service performed surgical lavage and wound closure and, subsequently, the spine surgery service implemented intravenous antibiotic therapy. During the follow-up visit that took place 20 days after surgery, there was evidence of improvement in the motor function of the lower limbs, voluntary contraction of the quadriceps muscles, muscle strength 1/5 on the Daniels scale in both legs, no sensory changes, and grade C ASIA. However, the patient still required bladder catheterization.
Discussion
Surgical management of gunshot wounds to the spine, although controversial, aims to maintain spinal stability, reduce neurological deficit, and prevent complications such as cerebrospinal fluid fistula and migration of the projectile.2,3,4 Physicians who favor conservative treatment of these wounds have reported cases of neurological recovery without projectile removal,5-8 while those who propose surgical management recommend early removal (within the first 24 to 48 hours) if the patient is stable,2,3,9-13 in order to prevent worsening of the health status and the appearance of new neurological symptoms and signs due to projectile migration, as well as meningitis, epidural fibrosis, intramedullary dystrophic calcification, and long-term effects of lead poisoning.12,14,15
It has been reported that patients in whom surgical removal of the projectile has been performed had partial or complete recovery of neurological symptoms.10,16-18 Furthermore, some authors have pointed out that early removal of the projectile from the spinal canal facilitates the neurological recovery of the patient since the axons in this region have the capacity to regenerate.2,12 It should be noted that only one of the studies found during the preparation of this article reported that the patient did not recover from the neurological deficit after removing the bullet.16
It has been described that projectiles that migrate usually lead to deterioration of neurological function and, therefore, migration is a criterion for surgery.20 Also, in patients with migration and intradural location of the projectile, it is recommended to perform surgery as soon as possible to prevent further damage to the patient, considering that Ghori et al.18 reported that a patient presented cauda equina syndrome 15 months after the bullet impact due to the migration of the bullet through the spinal canal.
The displacement of these migrating intradural projectiles during surgery was reported in the articles found and reviewed, but that event is expected in these cases. In the present case report, laminectomy was performed in the sacral region based on the results of preoperative imaging tests since the projectile was not found during this procedure. Consequently, fluoroscopy was used, which allowed observing cephalic migration of the bullet, making it necessary to extend the laminectomy to L4-L5; this is in line with the reports by Baldawa et al.19 In this sense, fluoroscopy should be performed before and during surgery to accurately locate the projectile and guide the laminectomy adequately.20 In addition, changes in patient position may help remove the projectile; in fact, the use of the reverse Trendelenburg position has been described to avoid further cephalic migration of the bullet.13,20
The present case has the particularity of involving the spinal cord in two sites, since the projectile that was extracted was initially lodged in the dural sac in the cauda equina and the second projectile was located in the abdomen, although it entered through the right paravertebral region at the level of L1, causing fracture of the pedicle and the right facet joint, with small vertebral fragments inside the spinal canal that were not susceptible to surgery. The incomplete spinal cord injury caused by the second projectile explains the initial grade A ASIA classification between T12-L1. Another relevant aspect is the improvement of motor function 20 days after surgery, achieving a grade A to C transition in ASIA.
Conclusions
Surgical treatment of gunshot wounds to the spine remains controversial. Migration of intrathecal projectiles may worsen neurological deficits and cause other short- or long-term complications, so surgical removal is recommended in these cases. The migration of these projectiles during surgery is common, and fluoroscopy should be used before and during the procedure. Moreover, proper positioning of the patient may facilitate the surgery.
Informed consent
The patient’s participation was voluntary, and his parents signed the informed consent form endorsing this case report. The confidentiality of the data obtained, as well as the identity of the subjects, was preserved at all times.
Conflicts of interest
None stated by the authors.
Funding
Acknowledgments
None stated by the authors.
References
1.Jaiswal M, Mittal RS. Concept of Gunshot Wound Spine. Asian Spine J. 2013;7(4):359-64. https://doi.org/gb94x4.
2.Sajid MI, Ahmad B, Mahmood SD, Darbar A. Gunshot injury to spine: An institutional experience of management and complications from a developing country. Chin J Traumatol. 2020;23(6):324-8. https://doi.org/jt66.
3.Aljuboori Z. Surgical removal of a spinal intrathecal projectile led to a significant improvement of cauda equina syndrome. Surg Neurol Int. 2020;11:227.https://doi.org/jt67.
4.Patil R, Jaiswal G, Gupta TK. Gunshot wound causing complete spinal cord injury without mechanical violation of spinal axis: Case report with review of literature. J Craniovertebr Junction Spine 2015;6(4):149-57. https://doi.org/jt69.
5.Bassani R, Morselli C, Agnoletto M, Brambilla L, Peretti GM. Management of gunshot wound to the lumbosacral spine in a 17-year-old girl without neurological impairment. J Biol Regul Homeost Agents. 2020;34(4 Suppl. 3):1-5.
6.Oktem IS, Selçuklu A, Kurtsoy A, Kavuncu IA, Paşaoğlu A. Migration of bullet in the spinal canal: a case report. Surg Neurol 1995;44:548-50. https://doi.org/czd5tt.
7.Rajan DK, Alcantara AL, Michael DB. Where’s the bullet? A migration in two acts. J Trauma 1997;43(4):716–8. https://doi.org/bd6m4h.
8.Morare N, Moeng MS. Unusual case of a migrating spinal bullet: An opportunity for reflection. Trauma Case Rep. 2020;27:100301. https://doi.org/jt7b,
9.Jun W, Yi-Jun K, Xiang-Sheng Z, Jing W. Cauda equina syndrome caused by a migrated bullet in dural sac. Turk Neurosurg. 2010;20(4):566-9. https://doi.org/d3tmp9.
10.Chan YT, Al-Mahfoudh R, Thennakon S, Eldridge P, Pillay R. Migrating intrathecal high-velocity projectile. Br J Neurosurg 2015;29(4):585-6. https://doi.org/jt7c.
11.Bordon G, Burguet Girona S. Gunshot wound in lumbar spine with intradural location of a bullet. Case Rep Orthop 2014;2014:698585. https://doi.org/gb9849.
12.Harsha KJ, Thomas A. Penetrating Injury to Cauda Equina from a Missile Fragment, Completely Recovered after Delayed Surgical Removal of Ballistic Fragment. Asian J Neurosurg. 2018;13(2):433-5. https://doi.org/gdfbxp.
13.Morrow KD, Podet AG, Spinelli CP, Lasseigne LM, Crutcher CL, Wilson JD,et al.. A case series of penetrating spinal trauma: comparisons to blunt trauma, surgical indications, and outcomes. Neurosurg Focus. 2019;46(3):E4. https://doi.org/jt7d.
14.Ryu B, Kim SB, Choi MK, Kim KD. Radiculopathy as delayed presentations of retained spinal bullet. J Korean Neurosurg Soc. 2015;58(4):393-6. https://doi.org/jt7f.
15.Todnem N, Hardigan T, Banerjee C, Alleyne CH Jr. Cephalad Migration of Intradural Bullet from Thoracic Spine to Cervical Spine. World Neurosurg. 2018;119:6-9. https://doi.org/gfmfvf.
16.Young WF Jr, Katz MR, Rosenwasser RH. Spontaneous migration of an intracranial bullet into the cervical canal. South Med J. 1993;86(5):557–9. https://doi.org/fsgz4b.
17.Ojukwu DI, Beutler T, Goulart CR, Galgano M. Bullet retrieval from the cauda equina after penetrating spinal injury: A case report and review of the literature. Surg Neurol Int. 2021;12:163. https://doi.org/jt7g.
18.Ghori SA, Khan MS, Bawany FI. Delayed cauda equina syndrome due to a migratory bullet. J Coll Physicians Surg Pak. 2014;24(Suppl 3):S219-20.
19.Baldawa S, Shivpuje V. Migratory low velocity intradural lumbosacral spinal bullet causing cauda equina syndrome: report of a case and review of literature. Eur Spine J. 2017;26(Suppl 1):128-35. https://doi.org/gbp3z6.
20.Siddiqui MI, Hawksworth SA, Sun DY. Removal of Migrating Lumbar Spine Bullet: Case Report and Surgical Video. World Neurosurg 2019;131:62-4. https://doi.org/jt7h.